| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Cardiology Examination (OSCE)
Related Subjects: |Breast Anatomy and Examination (OSCE) |Shoulder examination(OSCE) |Testicular examination(OSCE) |Hernia Examination (OSCE) |Rectal examination (OSCE) |Liver Examination (OSCE) |Cerebellar Examination (OSCE) |Upper and Lower Limb Neurology (OSCE) |Gastroenterology Examination (OSCE) |Respiratory Examination (OSCE) |Cardiology Examination (OSCE)
🔍 A cardiac exam is an active process — always think and look for signs systematically rather than waiting for them to appear.
| 🫁 Cardiology Exam: Overall Plan |
|---|
|
💡 Exam Pearls
• Always state BP would be measured. • Add “I’d like to complete with fundoscopy, urine dip, ECG & echo.” • JVP is best seen with tangential light. • Clubbing + splinter haemorrhages + new murmur = think infective endocarditis. • Always compare both sides: pulses, auscultation areas.
🫀 Complete Cardiac Examination OSCE Guide
👉 The cardiac exam is an active process — you must think, look, and integrate findings systematically. This article combines structured steps, teaching pearls, common findings, and a rapid-revision checklist into one complete resource.
🔑 Principles
- Follow a clear sequence: Inspection → Palpation → Auscultation → Special Maneuvers → Peripheral Signs → Closure.
- Always communicate with the patient and maintain dignity.
- Finish by stating how you’d complete the exam (BP, fundoscopy, urine dipstick, ECG, echo).
- Examiner tip: Talk through your steps. If you forget to do something, verbalising still gains marks. <
1️⃣ Preparation
- 🧼 Wash hands
- 👋 Introduce yourself & confirm patient ID
- 📝 Explain exam, obtain consent
- 🛏️ Position: semi-recumbent (45°), expose chest to waist while maintaining dignity
2️⃣ General Inspection (End of Bed 👀)
- Patient: distress, breathlessness, cyanosis, pallor, cachexia
- Environment: oxygen, nebulisers, GTN spray, IV fluids, ECG leads, mobility aids
- Bedside clues: urine pot (haematuria), sputum pot, fluid balance charts
3️⃣ Hands & Arms ✋
- Inspection: clubbing, splinter haemorrhages, Osler’s nodes, Janeway lesions, tendon xanthomata
- Pulses:
- Rate & rhythm (AF → irregularly irregular)
- Character: 🐢 Slow-rising → AS
| 💧 Collapsing → AR
- Radio-radial delay → subclavian stenosis
- Radio-femoral delay → coarctation of aorta
- BP measurement (mention both arms)
4️⃣ Face & Neck 🙂 & Eyes 👁️
- Eyes: xanthelasma, corneal arcus, conjunctival pallor, Roth spots
- Mouth: cyanosis, poor dentition
- Conjunctival pallor (anaemia), central cyanosis (lips, tongue).
- Xanthelasma / corneal arcus → hyperlipidaemia.
- Malar flush → mitral stenosis. Down’s/Turner’s/Marfan’s facies (syndromic associations).
- Neck: JVP at 45°, hepatojugular reflux, carotid pulse (one side at a time), listen for bruits
Hands ✋
- Clubbing → congenital cyanotic heart disease, endocarditis.
- Splinter haemorrhages, Osler’s nodes, Janeway lesions → endocarditis.
- Nicotine staining, tendon xanthomata, arachnodactyly, joint hypermobility (Marfan/Ehlers-Danlos).
- Temperature (warm/cold), perfusion.
Pulse & Rhythm ❤️
- Rate (brady <60, tachy >100). Count for 15s or full minute if irregular.
- Rhythm: regular / irregularly irregular (AF) / regularly irregular (ectopics, Mobitz II).
- Character: collapsing (AR), slow-rising (AS), jerky (HOCM), bisferiens (mixed AR/AS).
- Compare both radials; check radiofemoral delay (coarctation).
Blood Pressure 💉
- Measure both arms if coarctation/dissection suspected.
- Pulse pressure: narrow (AS), wide (AR, thyrotoxicosis).
5️⃣ Chest Inspection 👕
- Scars: sternotomy, lateral thoracotomy, ICD/PPM bulge
- Deformities: pectus excavatum, scoliosis
- Visible pulsations
- Pacemaker scars (usually L infraclavicular).
6️⃣ Palpation 🤲
- Apex beat: site, size, character, displacement
- Heaves: RV hypertrophy
- Thrills: palpable murmurs
7️⃣ Auscultation 🎧
- Areas (use diaphragm + bell):
- 🔴 Aortic → 2nd ICS, RSB
- 🔵 Pulmonary → 2nd ICS, LSB
- 🟢 Tricuspid → 4th ICS, LSE
- 🟣 Mitral (apex) → 5th ICS, MCL
- Axilla → MR radiation
- Carotids → AS radiation (after bruit check)
- Listen for:
- S1 & S2 clarity
- Extra sounds: 💧 S3 (HF, overload), 🔔 S4 (stiff LV)
- Murmurs: systolic, diastolic, timing, radiation
- Pericardial rub: scratchy, triphasic
8️⃣ Special Maneuvers ⚡
- Valsalva → ↑ HOCM murmur
- Handgrip → ↑ MR & AR murmurs
- Left lateral decubitus → accentuates MS, S3
- Sit forward + expiration → accentuates AR
9️⃣ Peripheral Signs 👣
- Lung bases → crackles (CCF)
- Sacrum & ankles → oedema
- Legs → saphenous vein harvest scars with sternotomy scar for CABG, varicosities
- Face → malar flush (MS), cyanosis
🔟 Closure 🙏
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
- Patient: distress, breathlessness, cyanosis, pallor, cachexia
- Environment: oxygen, nebulisers, GTN spray, IV fluids, ECG leads, mobility aids
- Bedside clues: urine pot (haematuria), sputum pot, fluid balance charts
3️⃣ Hands & Arms ✋
- Inspection: clubbing, splinter haemorrhages, Osler’s nodes, Janeway lesions, tendon xanthomata
- Pulses:
- Rate & rhythm (AF → irregularly irregular)
- Character: 🐢 Slow-rising → AS
| 💧 Collapsing → AR
- Radio-radial delay → subclavian stenosis
- Radio-femoral delay → coarctation of aorta
- BP measurement (mention both arms)
4️⃣ Face & Neck 🙂 & Eyes 👁️
- Eyes: xanthelasma, corneal arcus, conjunctival pallor, Roth spots
- Mouth: cyanosis, poor dentition
- Conjunctival pallor (anaemia), central cyanosis (lips, tongue).
- Xanthelasma / corneal arcus → hyperlipidaemia.
- Malar flush → mitral stenosis. Down’s/Turner’s/Marfan’s facies (syndromic associations).
- Neck: JVP at 45°, hepatojugular reflux, carotid pulse (one side at a time), listen for bruits
Hands ✋
- Clubbing → congenital cyanotic heart disease, endocarditis.
- Splinter haemorrhages, Osler’s nodes, Janeway lesions → endocarditis.
- Nicotine staining, tendon xanthomata, arachnodactyly, joint hypermobility (Marfan/Ehlers-Danlos).
- Temperature (warm/cold), perfusion.
Pulse & Rhythm ❤️
- Rate (brady <60, tachy >100). Count for 15s or full minute if irregular.
- Rhythm: regular / irregularly irregular (AF) / regularly irregular (ectopics, Mobitz II).
- Character: collapsing (AR), slow-rising (AS), jerky (HOCM), bisferiens (mixed AR/AS).
- Compare both radials; check radiofemoral delay (coarctation).
Blood Pressure 💉
- Measure both arms if coarctation/dissection suspected.
- Pulse pressure: narrow (AS), wide (AR, thyrotoxicosis).
5️⃣ Chest Inspection 👕
- Scars: sternotomy, lateral thoracotomy, ICD/PPM bulge
- Deformities: pectus excavatum, scoliosis
- Visible pulsations
- Pacemaker scars (usually L infraclavicular).
6️⃣ Palpation 🤲
- Apex beat: site, size, character, displacement
- Heaves: RV hypertrophy
- Thrills: palpable murmurs
7️⃣ Auscultation 🎧
- Areas (use diaphragm + bell):
- 🔴 Aortic → 2nd ICS, RSB
- 🔵 Pulmonary → 2nd ICS, LSB
- 🟢 Tricuspid → 4th ICS, LSE
- 🟣 Mitral (apex) → 5th ICS, MCL
- Axilla → MR radiation
- Carotids → AS radiation (after bruit check)
- Listen for:
- S1 & S2 clarity
- Extra sounds: 💧 S3 (HF, overload), 🔔 S4 (stiff LV)
- Murmurs: systolic, diastolic, timing, radiation
- Pericardial rub: scratchy, triphasic
8️⃣ Special Maneuvers ⚡
- Valsalva → ↑ HOCM murmur
- Handgrip → ↑ MR & AR murmurs
- Left lateral decubitus → accentuates MS, S3
- Sit forward + expiration → accentuates AR
9️⃣ Peripheral Signs 👣
- Lung bases → crackles (CCF)
- Sacrum & ankles → oedema
- Legs → saphenous vein harvest scars with sternotomy scar for CABG, varicosities
- Face → malar flush (MS), cyanosis
🔟 Closure 🙏
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
- Rate & rhythm (AF → irregularly irregular)
- Character: 🐢 Slow-rising → AS | 💧 Collapsing → AR
- Radio-radial delay → subclavian stenosis
- Radio-femoral delay → coarctation of aorta
- Eyes: xanthelasma, corneal arcus, conjunctival pallor, Roth spots
- Mouth: cyanosis, poor dentition
- Conjunctival pallor (anaemia), central cyanosis (lips, tongue).
- Xanthelasma / corneal arcus → hyperlipidaemia.
- Malar flush → mitral stenosis. Down’s/Turner’s/Marfan’s facies (syndromic associations).
- Neck: JVP at 45°, hepatojugular reflux, carotid pulse (one side at a time), listen for bruits
Hands ✋
- Clubbing → congenital cyanotic heart disease, endocarditis.
- Splinter haemorrhages, Osler’s nodes, Janeway lesions → endocarditis.
- Nicotine staining, tendon xanthomata, arachnodactyly, joint hypermobility (Marfan/Ehlers-Danlos).
- Temperature (warm/cold), perfusion.
Pulse & Rhythm ❤️
- Rate (brady <60, tachy >100). Count for 15s or full minute if irregular.
- Rhythm: regular / irregularly irregular (AF) / regularly irregular (ectopics, Mobitz II).
- Character: collapsing (AR), slow-rising (AS), jerky (HOCM), bisferiens (mixed AR/AS).
- Compare both radials; check radiofemoral delay (coarctation).
Blood Pressure 💉
- Measure both arms if coarctation/dissection suspected.
- Pulse pressure: narrow (AS), wide (AR, thyrotoxicosis).
5️⃣ Chest Inspection 👕
- Scars: sternotomy, lateral thoracotomy, ICD/PPM bulge
- Deformities: pectus excavatum, scoliosis
- Visible pulsations
- Pacemaker scars (usually L infraclavicular).
6️⃣ Palpation 🤲
- Apex beat: site, size, character, displacement
- Heaves: RV hypertrophy
- Thrills: palpable murmurs
7️⃣ Auscultation 🎧
- Areas (use diaphragm + bell):
- 🔴 Aortic → 2nd ICS, RSB
- 🔵 Pulmonary → 2nd ICS, LSB
- 🟢 Tricuspid → 4th ICS, LSE
- 🟣 Mitral (apex) → 5th ICS, MCL
- Axilla → MR radiation
- Carotids → AS radiation (after bruit check)
- Listen for:
- S1 & S2 clarity
- Extra sounds: 💧 S3 (HF, overload), 🔔 S4 (stiff LV)
- Murmurs: systolic, diastolic, timing, radiation
- Pericardial rub: scratchy, triphasic
8️⃣ Special Maneuvers ⚡
- Valsalva → ↑ HOCM murmur
- Handgrip → ↑ MR & AR murmurs
- Left lateral decubitus → accentuates MS, S3
- Sit forward + expiration → accentuates AR
9️⃣ Peripheral Signs 👣
- Lung bases → crackles (CCF)
- Sacrum & ankles → oedema
- Legs → saphenous vein harvest scars with sternotomy scar for CABG, varicosities
- Face → malar flush (MS), cyanosis
🔟 Closure 🙏
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
- Apex beat: site, size, character, displacement
- Heaves: RV hypertrophy
- Thrills: palpable murmurs
7️⃣ Auscultation 🎧
- Areas (use diaphragm + bell):
- 🔴 Aortic → 2nd ICS, RSB
- 🔵 Pulmonary → 2nd ICS, LSB
- 🟢 Tricuspid → 4th ICS, LSE
- 🟣 Mitral (apex) → 5th ICS, MCL
- Axilla → MR radiation
- Carotids → AS radiation (after bruit check)
- Listen for:
- S1 & S2 clarity
- Extra sounds: 💧 S3 (HF, overload), 🔔 S4 (stiff LV)
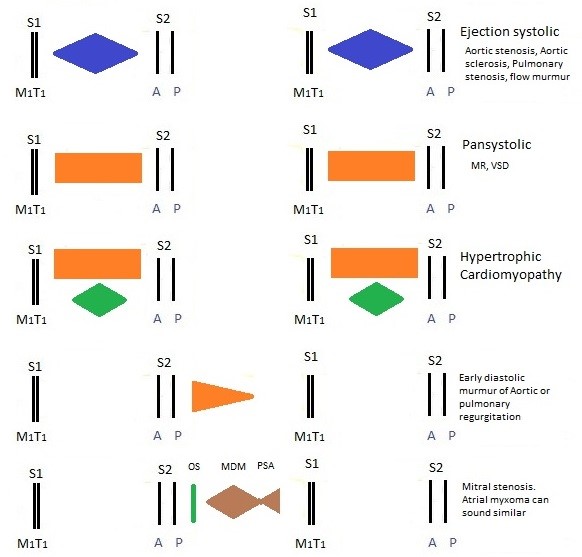
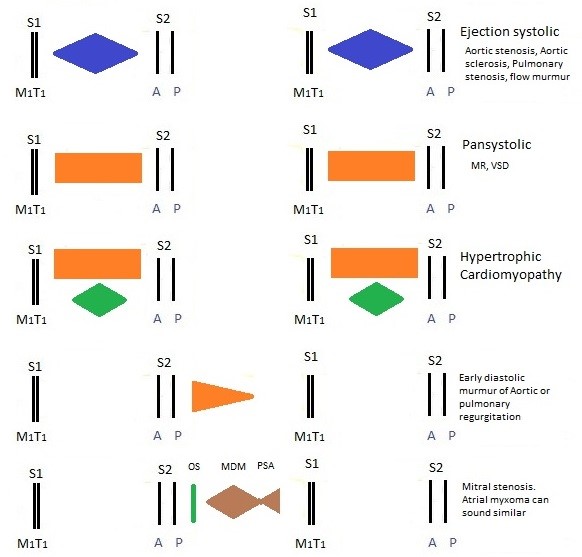
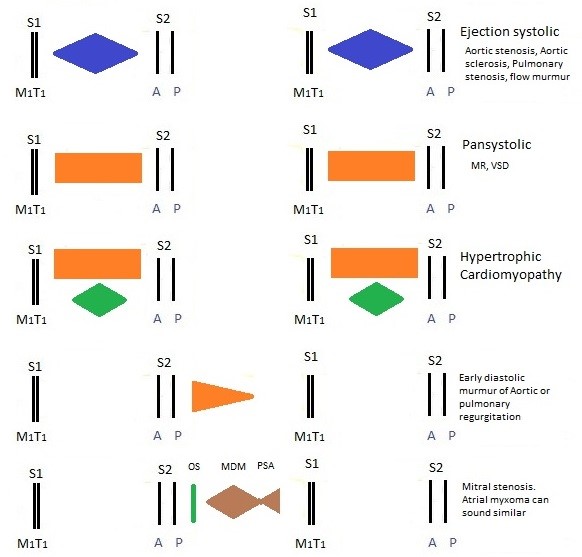
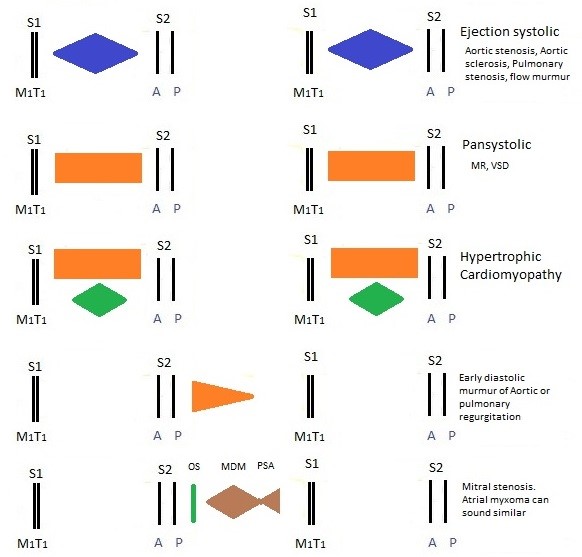
- Murmurs: systolic, diastolic, timing, radiation
- Pericardial rub: scratchy, triphasic
8️⃣ Special Maneuvers ⚡
- Valsalva → ↑ HOCM murmur
- Handgrip → ↑ MR & AR murmurs
- Left lateral decubitus → accentuates MS, S3
- Sit forward + expiration → accentuates AR
9️⃣ Peripheral Signs 👣
- Lung bases → crackles (CCF)
- Sacrum & ankles → oedema
- Legs → saphenous vein harvest scars with sternotomy scar for CABG, varicosities
- Face → malar flush (MS), cyanosis
🔟 Closure 🙏
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
- 🔴 Aortic → 2nd ICS, RSB
- 🔵 Pulmonary → 2nd ICS, LSB
- 🟢 Tricuspid → 4th ICS, LSE
- 🟣 Mitral (apex) → 5th ICS, MCL
- Axilla → MR radiation
- Carotids → AS radiation (after bruit check)
- S1 & S2 clarity
- Extra sounds: 💧 S3 (HF, overload), 🔔 S4 (stiff LV)
- Murmurs: systolic, diastolic, timing, radiation
- Pericardial rub: scratchy, triphasic
- Valsalva → ↑ HOCM murmur
- Handgrip → ↑ MR & AR murmurs
- Left lateral decubitus → accentuates MS, S3
- Sit forward + expiration → accentuates AR
9️⃣ Peripheral Signs 👣
- Lung bases → crackles (CCF)
- Sacrum & ankles → oedema
- Legs → saphenous vein harvest scars with sternotomy scar for CABG, varicosities
- Face → malar flush (MS), cyanosis
🔟 Closure 🙏
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
- Thank patient, assist redressing
- Wash hands again
- Present findings
- State further steps: BP (both arms), fundoscopy, urine dipstick, ECG, echo
Present your findings clearly: “This patient has an ejection systolic murmur loudest in the aortic area, radiating to the carotids, with a slow-rising pulse and narrow pulse pressure — consistent with severe aortic stenosis.” Examiner tip: Even if unsure, structure + reasoning = marks.
💡 Teaching Pearls
• State missing steps you’d add (ECG, echo, fundoscopy, urine dip). • JVP is measured in cm above the sternal angle. • Always comment on scars and environment clues. • Clubbing + splinter haemorrhages + new murmur → think endocarditis. • A collapsing pulse is best felt by raising the arm above the head. • In OSCEs: “I’d like to complete the exam with BP, fundoscopy, urine dip, ECG, echo.” = ✅ marks.
📊 Common Cardiac Examination Findings (Master Table)
| Finding | Description | Technique | Clinical Significance |
|---|---|---|---|
| 🫀 Normal S1 & S2 | Crisp closure of AV & semilunar valves | Auscultation at all standard areas | Normal cardiac function |
| 🔀 Physiological split S2 | Inspiration delays P2 closure | Pulmonary area during inspiration/expiration | Normal; fixed split → ASD |
| 🎵 Systolic murmur | Harsh/blowing/ musical during systole | Auscultate; use maneuvers | Aortic stenosis, Mitral regurgitation, VSD |
| 🎶 Diastolic murmur | Low-pitched rumble | Bell at apex in LLDP | Mitral stenosis, Aortic regurgitation |
| 💧 S3 | Early diastolic sound during rapid filling | Bell at apex in LLDP | Heart failure, volume overload |
| 🔔 S4 | Late diastolic sound before S1 | Bell at apex (supine) | Stiff LV (HTN, IHD) |
| 🔊 Pericardial rub | Scratchy, triphasic sound | Lean forward, breath held | Acute pericarditis |
| ⚙️ Continuous murmur | “Machinery” quality throughout cycle | L infraclavicular area | Patent ductus arteriosus |
| ✋ Collapsing pulse | Bounding upstroke, rapid collapse | Palpate radial while raising arm | Aortic regurgitation, PDA, hyperdynamic states |
| 🐢 Slow-rising pulse | Gradual carotid upstroke | Palpate carotid pulse | Aortic stenosis |
Additional Information
🫀 Cardiovascular Examination: High-Yield Signs, Pulses & Murmurs
Mentor’s tip: anchor your exam to a structured sequence (look ➝ feel ➝ listen ➝ manoeuvres). Correlate each finding with haemodynamics and a differential. Small extra manoeuvres (e.g., handgrip, leaning forward) massively increase diagnostic yield.
👀 General Findings & Likely Causes
| Finding | Appearance | Possible Causes |
|---|---|---|
| Central/Peripheral Cyanosis 💙 | Bluish lips/tongue (central) or nailbeds (peripheral) | Congenital cyanotic heart disease, severe LV failure, pulmonary HTN, hypoxaemia, shunts (Eisenmenger) |
| Clubbing ☁️ | Loss of nailfold angle; spongy nailbed | Infective endocarditis, cyanotic CHD; (non-cardiac: bronchiectasis, lung Ca, IBD) |
| Splinter haemorrhages 🔴 | Longitudinal nail bed streaks | Infective endocarditis, vasculitis, trauma |
| Janeway lesions / Osler nodes / Roth spots 🦠 | Painless palms/soles macules; painful pulp nodules; retinal haemorrhages | Infective endocarditis |
| Jaundice 🟡 | Yellow sclerae/skin | Congestive hepatopathy (RHF), haemolysis (IE) |
| Peripheral oedema 🦶 | Pitting ankle/leg swelling | RHF, venous insufficiency, nephrotic syndrome; drugs (CCBs) |
| JVP ↑ / Distended neck veins 🪜 | Raised venous column, abnormal waves | RHF, TR (giant v), tamponade (y descent blunted), constrictive pericarditis (prominent y), SVC obstruction |
| Hepatomegaly ± Ascites 🫁 | Liver edge below costal margin; shifting dullness | RHF, TR, constriction; “cardiac cirrhosis” |
| Cachexia ⚖️ | Weight loss, muscle wasting | Advanced HF, chronic IE, malignancy |
| Palmar erythema ✋ | Red palms | Chronic liver disease (from HF), IE, pregnancy, thyrotoxicosis |
🖐️ Pulses: What They Tell You
| Pulse | Characteristics | Associated Conditions |
|---|---|---|
| Normal | Regular rate & amplitude | Physiological |
| Bounding / “Water-hammer” 🚰 | Collapsing, wide pulse pressure | Aortic regurgitation (Corrigan), PDA, thyrotoxicosis, fever, pregnancy |
| Thready 🪡 | Weak, rapid | Shock, severe hypovolaemia, advanced HF |
| Pulsus paradoxus 🎭 | SBP drop >10 mmHg on inspiration | Tamponade, severe asthma/COPD, constrictive pericarditis |
| Pulsus alternans ↕️ | Alternating strong/weak beats | Severe LV systolic failure |
| Bisferiens 〰️ | Two systolic peaks (carotid) | AR with AS, HOCM |
| Parvus et tardus 🐢 | Slow-rising, low amplitude | Severe aortic stenosis |
| Bigeminus ♾️ | Couplets; compensatory pause | Ventricular ectopy, digoxin effect/toxicity |
| Pulse deficit ➖ | Apical > radial rate | Atrial fibrillation, frequent ectopy |
| Radio-femoral delay ⏱️ | Femoral later than radial | Coarctation of the aorta |
🧪 JVP & Special Venous Signs (Bedside Hemodynamics)
| Sign | How to Elicit | Interpretation |
|---|---|---|
| Hepatojugular reflux | Firm RUQ pressure 10–15s | ≥3 cm sustained rise in JVP ➝ RV failure / poor reserve |
| Kussmaul’s sign | JVP rises on inspiration | Constrictive pericarditis, RV infarct, restrictive CM |
| Large ‘v’ waves | Visual venous waveform | Tricuspid regurgitation |
🔊 Heart Sounds & Extra Clues
| Sound | Features | Associations |
|---|---|---|
| S3 (“ventricular gallop”) | Early diastole, low-pitched | Volume overload: HF, MR, AR (can be normal <40y) |
| S4 (“atrial kick”) | Late diastole, before S1 | Stiff ventricle: AS, HOCM, HTN; absent in AF |
| Opening snap | After S2 | Mitral stenosis (shorter A2-OS = more severe) |
🎧 Murmurs: Sites, Timing, Manoeuvres
| Murmur | Best Site | Timing | Key Clinical Features | Manoeuvres (↑ / ↓) |
|---|---|---|---|---|
| Aortic Stenosis | R 2nd ICS | Systolic ejection | Harsh crescendo–decrescendo; radiates to carotids; narrow pulse pressure; parvus et tardus; angina/syncope/HF | ↑ with squat/leg raise; ↓ with Valsalva/standing |
| Mitral Regurgitation | Apex | Holosystolic | Blowing; to axilla; LA dilatation, AF, pulmonary congestion | ↑ with handgrip; ↑ in left lateral; ↓ with standing |
| Aortic Regurgitation | L 3rd/4th ICS | Early diastolic decrescendo | Best leaning forward at end-expiration; wide PP, collapsing pulse; de Musset; Quincke; may have Austin-Flint at apex | ↑ with handgrip; ↓ with amyl nitrite/vasodilation |
| Mitral Stenosis | Apex | Mid-diastolic rumble | Loud S1 + opening snap; left lateral position; signs of pulmonary HTN, AF, haemoptysis | ↑ with exercise/raising legs; ↓ with tachycardia resolution |
| Tricuspid Regurgitation | LLSB | Holosystolic | ↑ with inspiration (Carvallo); JVP v-waves; RHF signs | ↑ Inspiration; ↓ Expiration/standing |
| Pulmonic Stenosis | L 2nd ICS | Systolic ejection | Harsh; to left shoulder; RV heave; cyanosis if severe | ↑ Inspiration; ↓ Valsalva |
| VSD | LLSB | Harsh holosystolic | Loud without radiation; large shunts ➝ HF, FTT in infants | ↑ Handgrip (↑ afterload); ↓ with vasodilation |
| PDA | Left infraclavicular | Continuous “machine-like” | Bounding pulses; wide PP; may cause HF/PAH | ↑ with handgrip; best in systole-diastole junction |
| HOCM (LVOT) | LLSB/apex | Crescendo systolic | Young pt; S4; may mimic AS but no carotid delay | ↑ Valsalva/standing; ↓ squat/handgrip |
🧑⚕️ Fast Bedside Sequence (Exam Savers)
- Measure BP in both arms (AS/AR; aortic dissection if discrepant).
- Check collapsing pulse (AR) and RR/femoral delay (coarctation).
- JVP at 45°, then HJR if borderline; inspect waveform.
- Apex beat (displaced = volume load; heave = pressure load).
- Listen: all areas + carotids; then targeted manoeuvres (expiration/lean forward for AR; LLDP for MS/MR).
- Lungs for crackles (pulmonary oedema) and periphery for oedema, sacral swelling.
🚩 Do-Not-Miss Pearls
- AF + murmur ➝ think MS/MR; anticoag as indicated.
- Fever + embolic signs (Janeway/Osler/Roth) ➝ IE work-up (3 × blood cultures pre-antibiotics, echo).
- Syncope + ejection murmur in elderly ➝ severe AS until proven otherwise.
- New diastolic murmur is always pathological.
Teaching note: tie the sound to the pressure/volume state. AS = pressure overload (thick LV, slow carotid upstroke). AR/MR = volume overload (displaced, hyperdynamic apex; wide PP in AR). Right-sided murmurs increase with inspiration.
📚 References & Further Reading
- Talley & O’Connor – Clinical Examination
- Geeky Medics OSCE Guides
- OSCEstop Resources
