| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Epiglottitis
🚨 Acute Epiglottitis is a rapidly progressive, life-threatening infection of the supraglottic structures that can cause sudden airway obstruction. ⚠️ Emergency: Immediate involvement of senior anaesthetic + ENT specialists is essential. 🛑 Do not attempt throat examination until the airway is secured – even minimal stimulation may precipitate complete obstruction.
ℹ️ About
- 🔥 Acute epiglottitis = cellulitis & inflammation of the epiglottis & aryepiglottic folds.
- 👶 Once a classic paediatric emergency, but 📈 adult incidence has risen due to Hib vaccination in children.
- 💉 In children, Hib immunisation reduced incidence >90%.
- ⚡ Mortality: ~1–5% overall, but higher in adults due to delayed recognition.
🦠 Aetiology
- Children (unvaccinated): Haemophilus influenzae type b.
- Adults: Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus aureus, Neisseria meningitidis.
- Risk factors:
- 🚫 No Hib vaccination.
- 🦠 Immunocompromised (HIV, chemo, steroids).
- 🍬 Diabetes mellitus.
- 🔥 Thermal/chemical injury (inhalation burns, caustics).
- 💊 Immunosuppressive medication.
🩺 Clinical Presentation
- ⏱️ Rapid onset (hours) – unlike croup which is gradual.
- Classic triad in children: 🤤 Drooling + 😰 Distress + 🗣️ Dysphonia ("3 Ds").
- Key features:
- 😖 Severe sore throat & odynophagia (disproportionate to oropharyngeal findings).
- 🗣️ Muffled “hot potato” voice ± hoarseness.
- 🌬️ Soft inspiratory stridor.
- 🤤 Drooling (inability to swallow).
- 🌡️ High fever >38.5°C + toxic appearance.
- 🧎 Tripod position: sitting forward, chin protruded, mouth open.
- 👶 Children often refuse to lie flat (risk of obstruction).
- Adults may present less dramatically – sore throat + dysphagia ± mild stridor → beware under-diagnosis.
🔬 Investigations (only after airway secured!)
- 🧪 FBC, CRP, blood cultures.
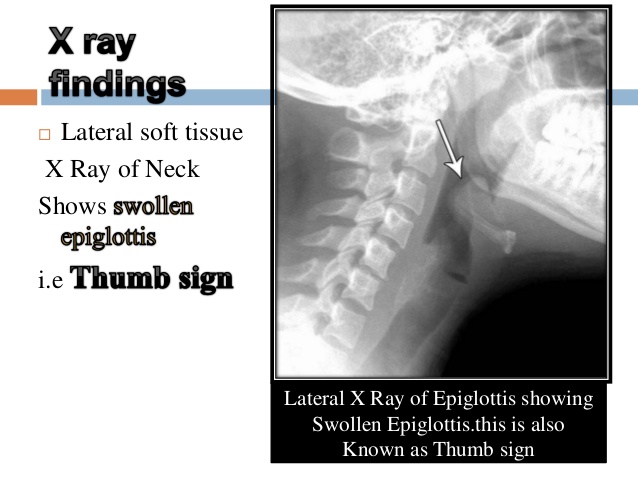
- 🖼️ Lateral neck X-ray: “Thumbprint sign” (swollen epiglottis). But do not delay airway intervention.
- 👁️ Fibre-optic laryngoscopy: diagnostic gold standard – only in controlled environment with airway backup.
📊 Comparison: Croup vs Bacterial Tracheitis vs Epiglottitis
| 🗣️ Croup | 🦠 Bacterial Tracheitis | 🚨 Epiglottitis | |
|---|---|---|---|
| Cause | Viral (parainfluenza) | Staph aureus, Strep spp. | Hib, others |
| Onset | Gradual (days) | Gradual → rapid | Sudden (hours) |
| Fever | Low-grade | High | High |
| Cough | Barking | Productive, purulent | Absent |
| Stridor | Inspiratory | Biphasic | Soft inspiratory |
| Swallowing | Normal | Painful | Drooling, painful |
| Posture | Lying OK | Variable | Tripod |
| Response | Good to steroids + nebulised adrenaline | Poor response | Urgent airway required |
🚑 Management
- Do not upset the child – avoid IV attempts, bloods, unnecessary handling.
- 💨 High-flow humidified O₂; keep upright & calm (with parent).
- 📞 Call ENT + anaesthetics + paediatrics immediately.
- Airway:
- ✅ Intubation in theatre by senior anaesthetist with ENT standby.
- 🔪 Surgical airway (cricothyrotomy/tracheostomy) if intubation fails.
- Medical therapy (post-airway):
- 💊 IV ceftriaxone or cefotaxime (empiric).
- ➕ Consider vancomycin/flucloxacillin if MRSA/S. aureus suspected.
- 💊 Corticosteroids sometimes used to reduce oedema (evidence mixed).
- 🧴 IV fluids & analgesia for support.
- Ongoing: ICU admission, close observation, remove ETT only when swelling resolved (usually 48–72 hrs).
- Prevention: Hib vaccination programme (key reason for reduced childhood cases).
✅ Key Pearls
- 🚨 Epiglottitis = airway emergency until proven otherwise.
- 🛑 Never use tongue depressor outside controlled theatre.
- 👶 Children: rapid deterioration likely → manage in PICU/ENT centre.
- 🧑 Adults: subtler onset → consider epiglottitis in severe sore throat with normal throat exam.
- 💉 Early Hib vaccination dramatically reduced paediatric incidence.
🎯 Exam/OSCE Tips
- Remember the “3 Ds” in kids: Drooling + Distress + Dysphonia.
- Tripod posture = ominous sign of impending obstruction.
- Airway first, antibiotics second → never delay airway for investigations.
- Differentiate from croup: no barking cough in epiglottitis.
Cases — Acute Epiglottitis (Children)
- Case 1 — Classic Hib presentation 🚨: A 4-year-old previously well boy presents with sudden high fever, drooling, muffled “hot potato” voice, and severe sore throat. He is sitting upright in tripod position, stridorous, and anxious. O₂ sats 90% on air. Diagnosis: acute epiglottitis (likely Hib in an unimmunised child). Managed with urgent anaesthetic/ENT team for controlled airway and IV ceftriaxone.
- Case 2 — Rapid deterioration 🕒: A 6-year-old girl develops sudden inspiratory stridor and severe respiratory distress after 12 hours of sore throat. She is pale, tachycardic, and refusing to lie down. Exam is limited due to risk of obstruction. Diagnosis: acute epiglottitis with impending airway obstruction. Managed with immediate anaesthetic-led airway stabilisation in theatre, oxygen, and IV antibiotics — avoid throat examination in ED.
- Case 3 — Post-vaccination rare case 💉: A 7-year-old boy (fully vaccinated) presents with fever, drooling, dysphagia, and soft inspiratory stridor. Swab later grows Streptococcus pyogenes. Diagnosis: epiglottitis due to non-Hib organism. Managed with airway protection, IV cefotaxime, and close PICU monitoring.
Teaching Point 🩺: Acute epiglottitis is a paediatric emergency caused by infection of the epiglottis (historically Hib, now rare with vaccination). Classic features: high fever, drooling, dysphagia, stridor, muffled voice, tripod posture. ⚠️ Do not attempt throat examination outside controlled environment → risk of complete airway obstruction. Management: secure airway (ENT/anaesthetics), IV antibiotics (ceftriaxone/cefotaxime), oxygen, supportive care. Prevention: Hib vaccination.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
