| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Wellens Syndrome
Related Subjects: |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |Acute Coronary Syndrome (ACS): Complications |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular STEMI |ACS: Sgarbossa Criteria |Wellen's syndrome
⚠️ Because Wellens syndrome patients have critical narrowing of the LAD coronary artery, stress testing is contraindicated. It may precipitate acute MI and sudden cardiac death.
🔎 Introduction
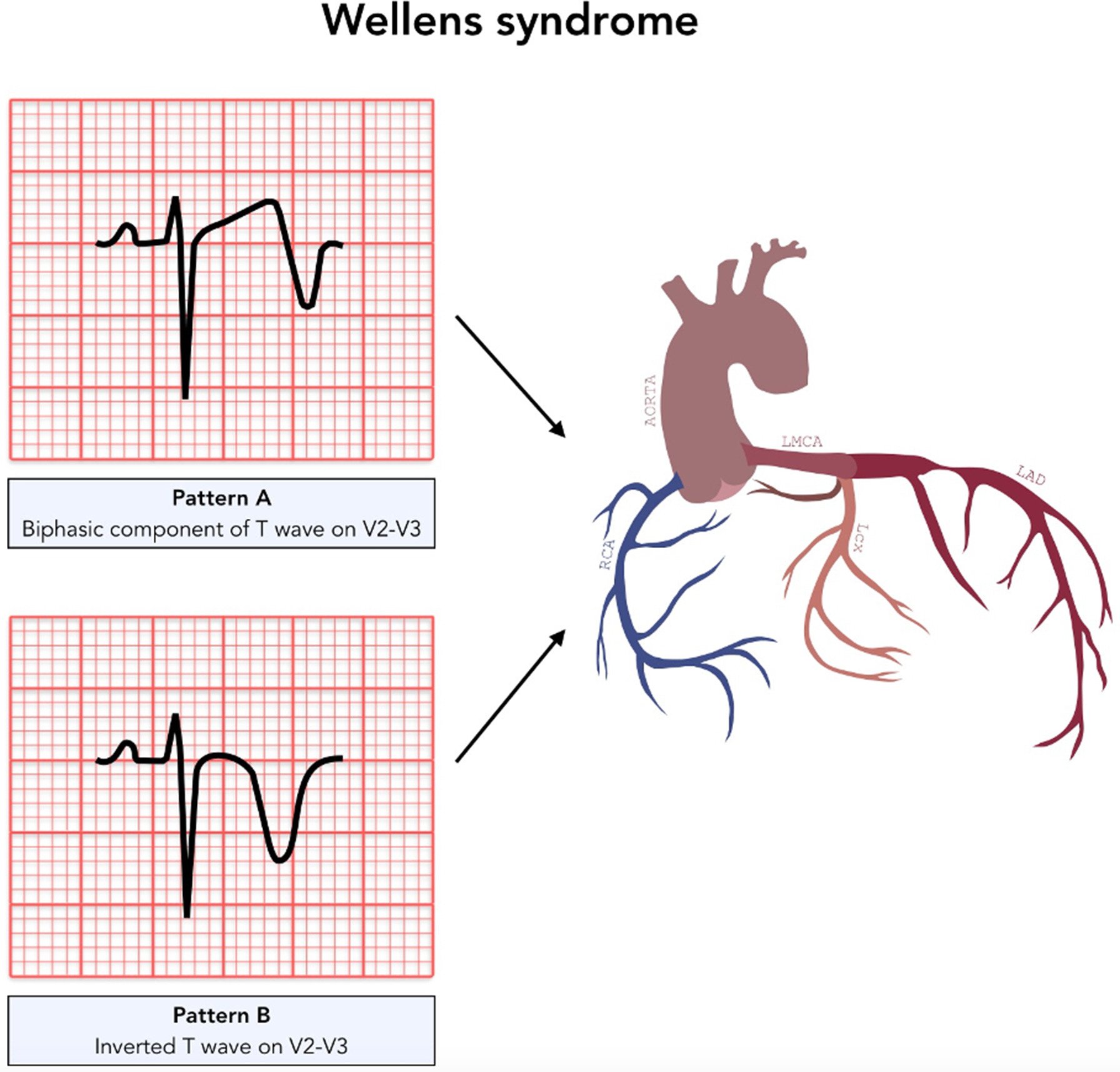
- Wellens syndrome = a classic ECG pattern indicating imminent anterior MI due to critical LAD stenosis.
- Key to recognise in the ED – early intervention is lifesaving.
🧬 Aetiology
- Represents >90% stenosis of the LAD artery.
- Critical narrowing → high risk of complete occlusion & anterior wall STEMI.
⚙️ Pathophysiology
- Atherosclerotic plaque: High-grade LAD lesion causes intermittent reduced perfusion.
- Vasospasm: LAD spasm may contribute to transient ischaemia.
- Increased demand: Exercise/stress raises oxygen demand, worsening ischaemia.
- Hypoxia: Systemic hypoxaemia aggravates LAD compromise.
⚠️ Risk Factors
- Diabetes mellitus
- Hypertension
- Hyperlipidaemia / Hypercholesterolaemia
- Smoking
- Metabolic syndrome
- Family history of premature IHD
- Age & occupational stress
🧾 Clinical Presentation
- Chest pain (often anginal, may have settled by time of ECG).
- Anginal equivalents: arm pain, jaw pain, dyspnoea.
- May be asymptomatic → ECG is crucial.
📊 Investigations
- Bloods: FBC, U&E, LFTs, lipids.
- Troponin: May be normal or only mildly raised.
- ECG hallmarks:
- Biphasic or deeply inverted T waves in V2–V3.
- Can extend V1–V6 (critical LAD territory).
- T wave normalisation + hyperacute waves = impending STEMI.
- Echocardiogram: Wall motion abnormalities in anterior wall.
- Coronary angiography: Gold standard for diagnosis & management planning.
🩺 Management
- Immediate Care: Admit CCU, oxygen if hypoxic, aspirin/clopidogrel, nitrates, beta-blockers (if not contraindicated).
- STEMI protocol: If ST elevation develops → manage as acute STEMI.
- Definitive: Early coronary angiography → PCI or CABG depending on anatomy.
- Avoid stress testing: Contraindicated due to risk of precipitating full infarct.
📌 Prognosis & Clinical Significance
- Untreated → very high risk of anterior wall MI within days to weeks.
- Early recognition + PCI/CABG = excellent outcome.
- Secondary prevention vital: BP & cholesterol control, diabetes optimisation, smoking cessation, antiplatelet + statin therapy.
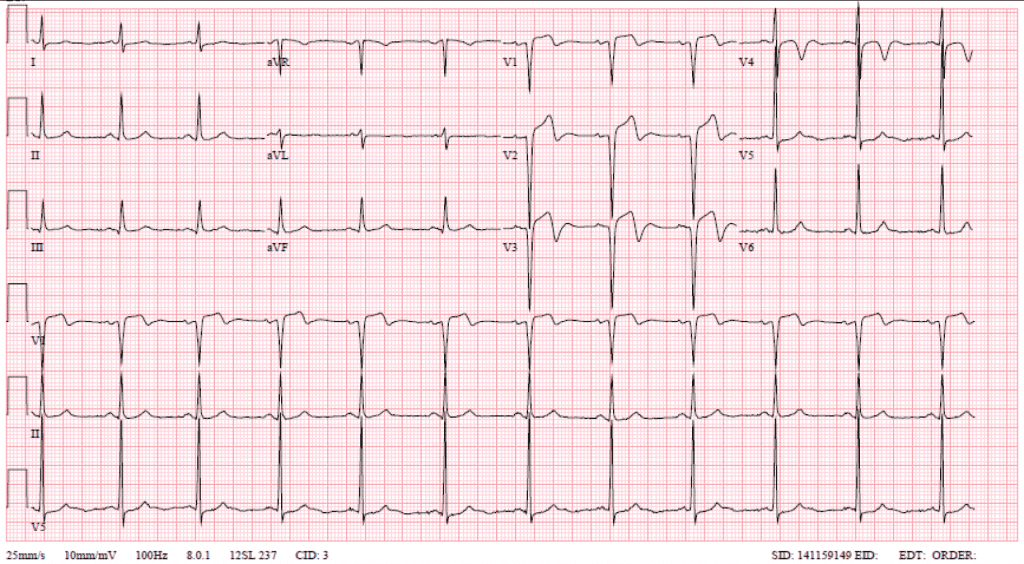
🖼️ Classic ECG Examples





📚 References
- Wellens Syndrome – NCBI Bookshelf
- de Zwaan C, Wellens HJ. “Characteristic electrocardiographic pattern indicating critical LAD stenosis.” Am Heart J. 1982.
Exam Pearl: – Wellens = T-wave changes in V2–V3 + critical LAD stenosis + pain-free at time of ECG. – Never stress test a Wellens patient 🚫🏃.
Cases — Wellens’ Syndrome
- Case 1 — Type A (biphasic T-waves) 📉: A 56-year-old man presents with intermittent central chest tightness over 2 days, now pain-free. ECG: biphasic T-waves in V2–V3, no ST elevation. Troponin mildly raised. Diagnosis: Wellens’ syndrome (critical LAD stenosis, Type A pattern). Managed with hospital admission, antiplatelets, and urgent coronary angiography ± PCI. ⚠️ Stress testing contraindicated due to risk of infarction.
- Case 2 — Type B (deeply inverted T-waves) ⚠️: A 63-year-old woman with diabetes presents with recent exertional angina, now pain-free in ED. ECG: deeply inverted, symmetrical T-waves in V2–V4, preserved R-wave progression. Troponin borderline. Diagnosis: Wellens’ syndrome (Type B pattern). Managed with dual antiplatelet therapy, heparin, and urgent revascularisation planning.
- Case 3 — Missed diagnosis → infarction 🚨: A 60-year-old man is discharged after presenting with atypical chest pain and “nonspecific T-wave changes.” Two days later he returns with severe chest pain. ECG: anterior ST-elevation MI. Angiography: complete proximal LAD occlusion. Retrospective review: prior ECG showed Wellens’ T-wave inversions. Diagnosis: progression of untreated Wellens’ syndrome to LAD infarction. Teaching point: always recognise the pattern!
Teaching Point 🩺: Wellens’ syndrome is a pre-infarction state caused by critical proximal LAD stenosis. ECG patterns (seen in pain-free state): - Type A: biphasic T-waves in V2–V3. - Type B: deeply inverted, symmetrical T-waves in anterior leads. No Q waves, no loss of R-wave progression, little ST elevation. ⚠️ High risk of extensive anterior MI → requires urgent angiography/PCI, not stress testing. Troponin may be normal or only mildly raised.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
