| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Haemorrhagic stroke
Related Subjects: |Subarachnoid Haemorrhage |Perimesencephalic Subarachnoid haemorrhage |Haemorrhagic stroke |Cerebellar Haemorrhage |Putaminal Haemorrhage |Thalamic Haemorrhage |ICH Classification and Severity Scores
🧠 Introduction
- Haemorrhagic stroke, also called Spontaneous Intracerebral Haemorrhage (SICH), is often sudden and devastating.
- Accounts for ~15% of all strokes (majority are ischaemic).
- One subtype is Subarachnoid Haemorrhage (SAH), usually from ruptured aneurysms or vascular anomalies (discussed separately).
- ⚠️ Mortality is high: 30–50% of patients with large bleeds die within 30 days.
- Smaller bleeds can have better outcomes → focus on identifying cause and preventing recurrence.
- ❌ Traumatic intracranial haemorrhage and extra-axial bleeds (subdural, extradural) are not classified as stroke.
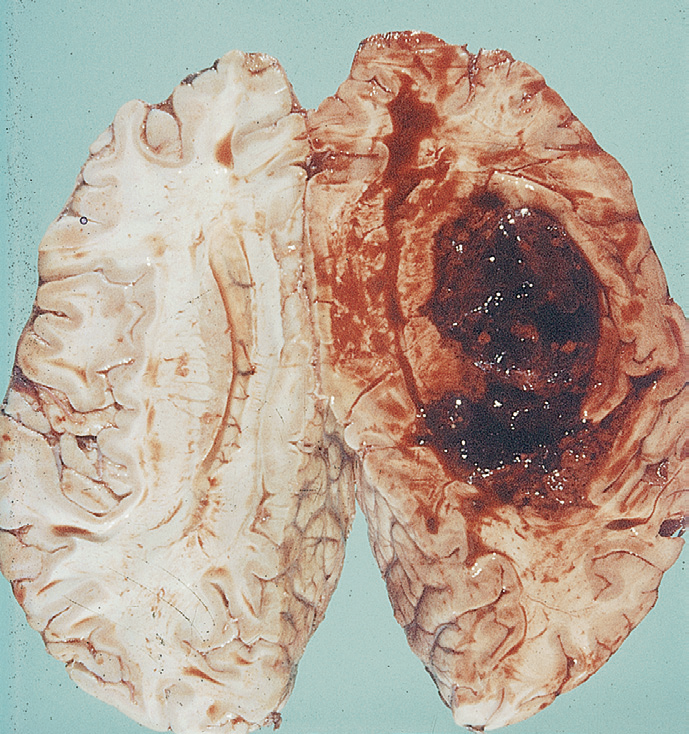
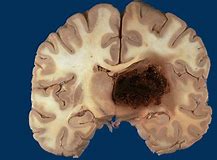
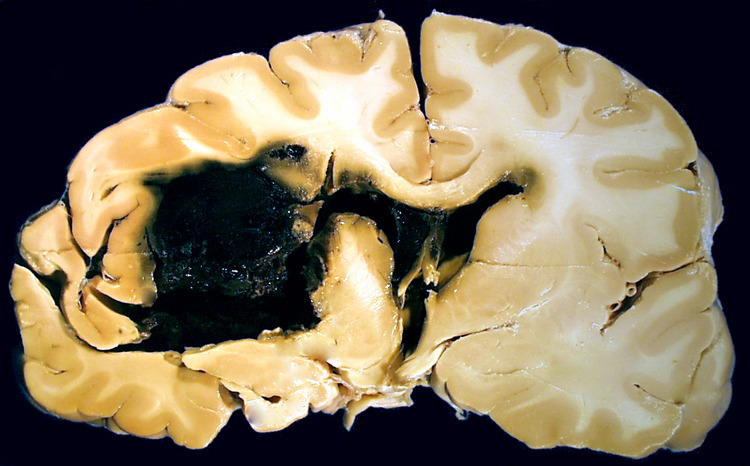
🔬 Pathological Appearance
On pathology and imaging, haemorrhagic strokes show destructive haematomas, surrounding oedema, and pressure effects:
⚙️ Aetiology
- Vessel rupture: Can occur anywhere from Circle of Willis arteries to small penetrating arterioles, capillaries, and draining veins.
- Aneurysms: Berry aneurysm rupture → high-pressure SAH.
- Small vessel disease: Hypertension → lipohyalinosis, Charcot–Bouchard microaneurysms → deep bleeds.
- Cerebral amyloid angiopathy: In elderly → lobar bleeds.
- Structural: AVMs, cavernomas, hereditary haemorrhagic telangiectasia.
- Neoplastic: Tumours (esp. melanoma, RCC, thyroid, choriocarcinoma, lung) prone to bleed.
- Coagulopathies: Anticoagulants (warfarin, DOACs), antiplatelets, thrombocytopenia, haemophilia, liver disease.
- Venous sinus thrombosis: Back-pressure haemorrhage → paradoxically requires anticoagulation.
🌍 Epidemiology
- More common in Afro-Caribbean, South-East Asian, and Japanese populations.
- Strong association with hypertension prevalence and genetic predisposition (amyloid angiopathy).
🧾 Causes by Age Group
- 🧓 Elderly: Hypertension, cerebral amyloid angiopathy.
- 👩 Younger adults: AVMs, aneurysms, cavernomas, coagulopathies.
- 💊 Any age: Anticoagulation therapy, illicit drugs (cocaine, amphetamines).
🧭 Types by Anatomy
- 🧠 Lobar: Cortex ± subcortical white matter.
- ⚫ Deep: Putaminal, thalamic, caudate, basal ganglia.
- 🧩 Brainstem: Pontine haemorrhage → sudden coma, pinpoint pupils.
- 🌀 Cerebellar: Ataxia, vertigo; large bleeds (>3 cm) may need evacuation.
- 💥 Subarachnoid haemorrhage: Usually aneurysmal.
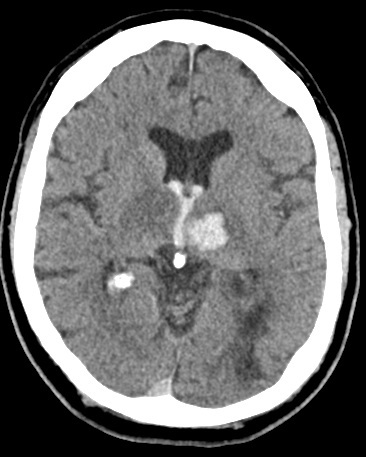
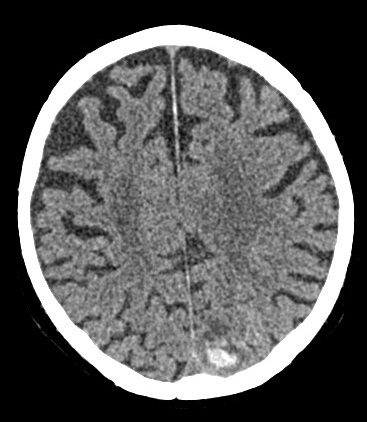
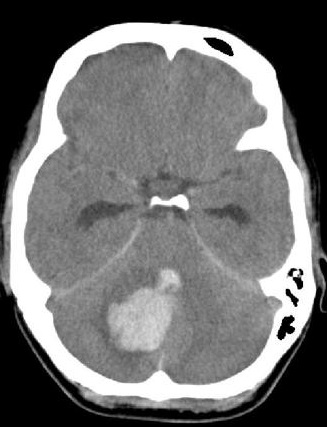
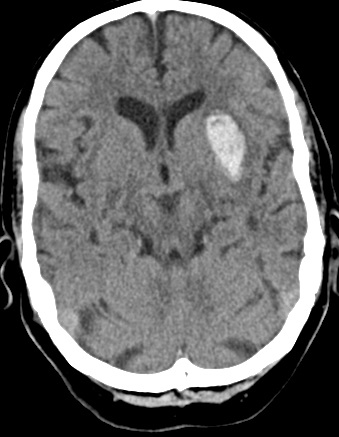
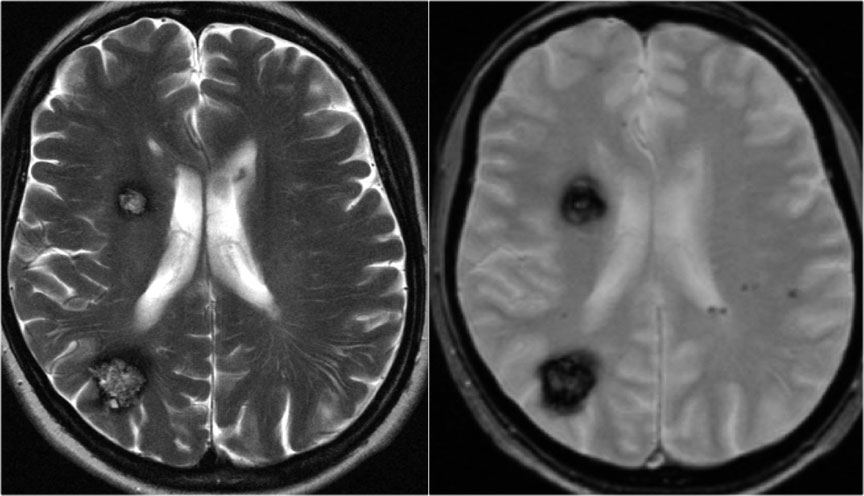
📸 Example Imaging
CT and MRI examples of haemorrhagic stroke:



🩺 Clinical Presentation
- 🧨 Sudden severe headache, vomiting, reduced consciousness.
- 🧑⚕️ Focal neurology: hemiparesis, hemisensory loss, aphasia, neglect, visual field deficits.
- 🌀 Cerebellar bleeds: vertigo, nausea, truncal ataxia, nystagmus.
- 🟣 Brainstem bleeds: coma, quadriplegia, miosis, “locked-in” syndrome.
- 🔦 SAH: Thunderclap headache, collapse, meningism, reduced GCS.
⚠️ Complications
- Intraventricular extension → acute deterioration, coma.
- Hydrocephalus from ventricular obstruction.
- Cerebral oedema, raised ICP, herniation (coning).
- Seizures (early or delayed).
- Rebleeding, especially in aneurysmal SAH and AVM.
🚩 Red Flags for Secondary Causes
- Age <50.
- No history of hypertension.
- Recurrent or atypical bleeds.
- Lobar location (esp. with soft tissue swelling or fracture → trauma vs primary bleed).
- Family history or features of inherited vascular syndromes (HHT).
🔍 Investigations
- 🩸 Bloods: FBC, U&E, LFT, glucose, coagulation, ESR/CRP.
- 🖼️ Non-contrast CT: First-line, detects haematoma, intraventricular blood, hydrocephalus.
- 🧲 MRI: Detects microbleeds, chronic haemosiderin, cavernomas (SWI/GRE).
- 📡 MRA/CTA: Aneurysms, AVMs, dissections.
- 🩻 MRV: Suspected venous sinus thrombosis.
- 📌 DSA: Gold standard for vascular malformations; small stroke risk.
- ❤️ Echocardiography: Endocarditis, embolic source.
- 💉 LP: For SAH if CT normal but suspicion high.
📊 Prognostic Scoring (ICH Score)
- GCS: 3–4 (+2), 5–12 (+1), 13–15 (0).
- Age ≥80: +1.
- Volume >30 ml: +1.
- Intraventricular haemorrhage: +1.
- Infratentorial location: +1.
➡️ Higher total = worse prognosis. 0 = 0%, 1 = 13%, 2 = 26%, 3 = 72%, 4 = 97%, 5 = 100% 30-day mortality.
⚖️ Management
- 🛑 Immediate: ABC, airway support, early CT, correct coagulopathy, cautious BP lowering, neurosurgical referral.
- 💊 Reverse anticoagulation: Warfarin INR>1.4 → Vit K + PCC (Octaplex). Stop DOAC/antiplatelets. Avoid platelets (PATCH trial).
- 📉 Blood pressure: Reduce to <160 systolic with IV agents (e.g. labetalol). Avoid hypoperfusion.
- 🧑⚕️ Neurosurgery: Consider clot evacuation, especially cerebellar bleeds >3 cm or deteriorating GCS. EVD for hydrocephalus.
- 💉 Seizure control: IV phenytoin/levetiracetam if seizures.
- 🧑🦽 Rehabilitation: MDT stroke/ICU team for survivors.
- ❌ Avoid: Routine mannitol (except bridging), steroids (harmful), unnecessary statin withdrawal without review.
📉 Prognosis
- Large bleeds, IVH, infratentorial location, and advanced age = worse outcomes.
- Many survivors are left with major neurological deficits.
💡 Exam Pearl: Intracerebral haemorrhage = sudden headache + neuro deficit + ↓ consciousness. ➡️ Early non-contrast CT is essential — clinical features alone cannot distinguish from ischaemic stroke.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
