| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Fever/Pyrexia of unknown origin (FUO PUO)
Related Subjects: | Fever in a Traveller | Malaria Falciparum | Malaria Non Falciparum | Viral Haemorrhagic Fevers (VHF) | Lassa Fever | Dengue | Marburg Virus Disease | AIDS/HIV | Yellow Fever | Ebola Virus | Leptospirosis | Crimean-Congo Haemorrhagic Fever | African Trypanosomiasis (Sleeping Sickness) | American Trypanosomiasis (Chagas Disease) | Incubation Periods | Notifiable Diseases UK
🌡️ Key Point: FUO requires multiple expert opinions because causes are broad, and not all prolonged fevers are infectious. Current definition: Documented fever persisting >2 weeks with no clear diagnosis despite thorough and directed investigation.
📖 About
- Original (Petersdorf & Beeson, 1960s): Temp >38.3 °C for >3 weeks with no diagnosis after 1 week of inpatient work-up (pre-CT/MRI era).
- Current: Fever >2 weeks with no diagnosis despite detailed investigations.
- Fever = cytokines/interferons reset hypothalamic set point. 🚨 May be absent in elderly, steroid-treated, or immunocompromised patients.
- Any pyrogen (microbial toxin, cytokine, necrotic material) can trigger fever.
🧾 Definitions
- Current: >2 weeks, unexplained after thorough testing.
- Original: >38 °C, >3 weeks, unexplained after 1 week hospital investigations.
🩺 Differential Diagnoses
- Infections: TB, endocarditis, urinary/resp tract infections.
- Abscesses: Pelvic, renal, epidural, subdiaphragmatic.
- Tropical/Parasitic: Malaria, amoebiasis, leishmaniasis, trypanosomiasis.
- Other infections: EBV/CMV, brucellosis, HIV, Lyme, Whipple’s, rickettsiae.
- Rheumatological: GCA, PMR, SLE, Still’s, vasculitides.
- Genetic: Familial Mediterranean Fever.
- Malignancy: Lymphoma, leukaemia, renal cell carcinoma, solid tumours.
- Other: Drug fever, atrial myxoma, thyrotoxicosis.
🔑 Key Clinical Approaches
- 🧳 History: travel, drug use (esp. IV), occupational & sexual exposures.
- 👀 Exam: skin, oral/dental, lymph nodes, rectal/pelvic where indicated.
- 📸 Imaging: chest X-ray, ultrasound, CT/MRI → hidden abscess/malignancy.
- 🔁 Re-evaluate: repeat history/exam frequently; new clues often evolve.
- 🤝 Seek early specialist input: rheumatology, haematology, microbiology, cardiology.
🔬 Investigations
- Basic labs: FBC, ESR/CRP, LFTs, U&Es, TFTs.
- Serology: EBV, CMV, HIV, Bartonella, Toxoplasma, Brucella, Lyme, Q fever.
- Microbiology: Blood, urine, stool cultures (≥3 sets); wound swabs if relevant.
- Imaging: CXR, abdo/pelvic US, CT, MRI. Consider bone/WBC-labelled scans.
- Specialised: Echocardiogram (endocarditis/myxoma), malaria films (×3), autoimmune panels (ANA, ANCA, RF).
- Biopsy: Liver (TB, lymphoma, granulomas), bone marrow (malignancy, leishmaniasis, TB), temporal artery (>50yrs, rule out GCA).
📊 Causes of FUO
| Category | Examples / Notes |
|---|---|
| 🦠 Common Infections (30–40%) | UTI, chest infections, endocarditis. Take blood cultures before antibiotics. |
| 🦟 Malaria | Travel history vital. Falciparum malaria = rapidly fatal. Do thick & thin films. |
| 🧫 Tuberculosis | Miliary/extrapulmonary. May need CXR, IGRA, biopsy. |
| 💥 Abscess | Splenic, perirenal, pelvic, spinal. Requires CT/US/MRI for localisation. |
| 🧬 Other Infections | HIV, osteomyelitis, typhoid, brucellosis, Lyme, EBV, CMV, Bartonella, toxoplasmosis. |
| 🎗️ Malignancy (~20%) | Lymphoma, leukaemia, renal cell carcinoma. Often ↑ESR/LDH. |
| 🔥 Inflammatory (10–20%) | GCA, Still’s, SLE, vasculitis, RA. Very high ESR in GCA. |
| ⚖️ Miscellaneous | Atrial myxoma, sarcoidosis, Crohn’s, FMF, occult haematoma, thyrotoxicosis. |
| ❓ Idiopathic | No diagnosis despite extensive work-up. |
| 💊 Drugs | Drug-induced fever; thorough med history crucial. |
| 🕵️ Factitious | Deliberate fever. Normal ESR/CRP. Check fresh urine temp to confirm. |
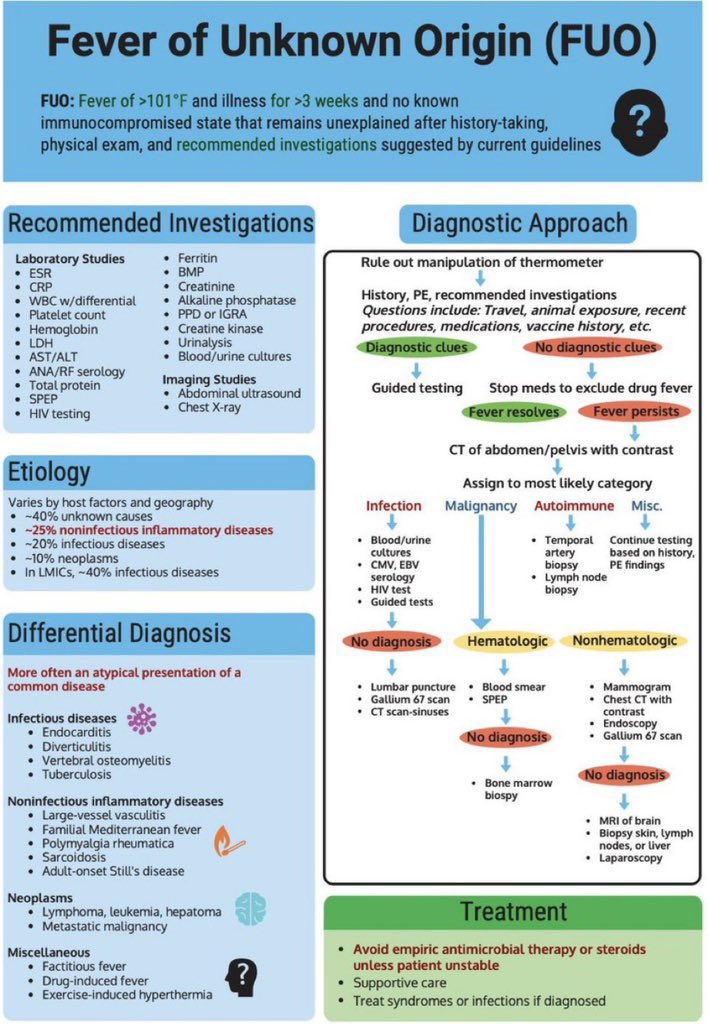 🧑⚕️ Management Principles
🧑⚕️ Management Principles
- 🚫 Avoid “blind” antibiotics - they obscure cultures & mask clues.
- ✅ Re-evaluate regularly; revisit history & exam with fresh eyes.
- 🤝 Discuss with seniors & specialists early (multidisciplinary approach).
- 📅 Stable outpatients: follow up carefully; unstable patients → urgent admission.
- 💊 Suspend unnecessary meds to rule out drug fever.
Cases - Pyrexia of Unknown Origin (PUO / FUO)
- Case 1 - Infective (Tuberculosis): A 35-year-old man presents with 6 weeks of intermittent fever, night sweats, and weight loss. No cough. CXR: miliary mottling. ESR raised, Quantiferon positive. Diagnosis: Disseminated tuberculosis. Management: Anti-TB therapy (RIPE regimen), prolonged course; notify public health.
- Case 2 - Infective (Endocarditis): A 52-year-old man with a prosthetic mitral valve presents with 5 weeks of low-grade fever, sweats, and weight loss. Exam: new murmur, splinter haemorrhages. Blood cultures: *Streptococcus viridans*. Echo: vegetation. Diagnosis: Infective endocarditis. Management: Prolonged IV antibiotics ± surgery if refractory or valve destruction.
- Case 3 - Malignancy (Lymphoma): A 42-year-old woman has 2 months of fever, drenching night sweats, and weight loss. Exam: cervical lymphadenopathy, splenomegaly. LDH high. Node biopsy: Reed–Sternberg cells. Diagnosis: Hodgkin lymphoma. Management: Staging and chemotherapy (ABVD regimen).
- Case 4 - Autoimmune (Adult-Onset Still’s Disease): A 28-year-old woman has daily spiking fevers, arthralgia, and a salmon-pink rash. Labs: neutrophilia, high ferritin, negative ANA/RF. Diagnosis: Adult-onset Still’s disease. Management: NSAIDs or corticosteroids; consider biologics if refractory.
- Case 5 - Autoimmune (Giant Cell Arteritis): A 70-year-old woman presents with fever, weight loss, new headache, and scalp tenderness. ESR 110 mm/hr. Temporal artery tender and thickened. Diagnosis: Temporal arteritis presenting as PUO. Management: High-dose corticosteroids immediately; confirm with temporal artery biopsy.
- Case 6 - Miscellaneous (Drug Fever): A 65-year-old man on long-term antibiotics for osteomyelitis develops persistent fever without focus. All cultures negative. Fevers stop 48 hours after stopping beta-lactam therapy. Diagnosis: Drug-induced PUO. Management: Stop culprit drug; supportive care.
Teaching Commentary 🌡️
PUO is defined as fever >38.3 °C on several occasions, lasting >3 weeks, with no diagnosis after 1 week of inpatient investigation. Causes fall into 4 groups: 1. Infections (TB, endocarditis, abscesses). 2. Malignancies (lymphoma, leukaemia, renal carcinoma). 3. Autoimmune/Inflammatory (GCA, Still’s disease, vasculitis, SLE). 4. Miscellaneous (drug fever, thyroiditis, sarcoidosis). Approach: repeat history/exam, serial blood cultures, imaging (CXR, CT, PET-CT), autoimmune panel, consider biopsy. Always review medications. Management is cause-specific - avoid empirical steroids/antibiotics until diagnosis unless patient is acutely unstable.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
