| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Uveitis
Related Subjects: |Episcleritis |Scleritis |Assessing a Red eye |Acute Angle Closure Glaucoma |Allergic and Infective Conjunctivitis |Anterior and Posterior Uveitis |Atropine Sulfate |Herpes simplex keratitis (HSK) |Acute Blepharitis |Chalazion
🍇 “Uveitis” comes from the Latin word uva, meaning grape. ⚠️ If there is recent intraocular surgery (e.g. cataract or intravitreal injections), always consider endophthalmitis as the cause of pain and photophobia.
📖 About
- 🔴 Inflammation of the uveal tract: iris, ciliary body, and choroid.
- ⚡ Causes include trauma, iatrogenic sources, infection, drugs, systemic autoimmune disease, or idiopathic.
- 👁️ Anterior uveitis often affects young adults and can cause long-term, sight-threatening complications.
📊 Epidemiology
- ~50% of cases are idiopathic.
- Can occur at any age, but peak ~40 years.
- Anterior uveitis = ~90% of cases.
🔎 Types
- Anterior uveitis: Iritis, cyclitis, or iridocyclitis.
- Posterior uveitis: Choroiditis, retinitis, chorioretinitis, or retinal vasculitis.
- Intermediate uveitis: Involves vitreous and peripheral retina.
- Panuveitis: Inflammation of the entire uveal tract.
🧬 Aetiology (50% idiopathic)
- Idiopathic anterior uveitis (often HLA-B27 positive).
- Trauma or ophthalmic surgery.
- Ocular syndromes: Fuchs’ heterochromic cyclitis, Posner–Schlossman syndrome.
- Rheumatology: Ankylosing spondylitis, Psoriatic arthritis, Reactive arthritis, JIA, Behçet’s, PAN, GPA (Wegener’s).
- Infective: HSV, VZV, CMV, TB, syphilis, toxoplasmosis, brucellosis, Lyme, leptospirosis.
- Systemic: Sarcoidosis, MS, Crohn’s, ulcerative colitis, Whipple’s disease.
- Rare: Primary CNS lymphoma.
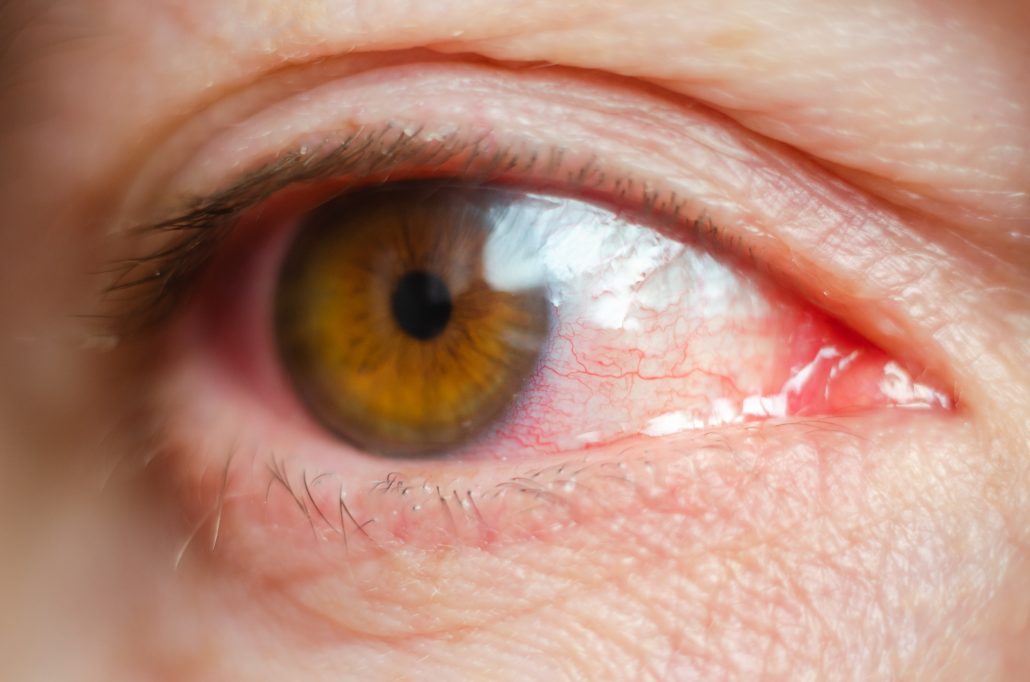
👁️ Clinical Features
- ⚡ Severe ocular pain, tearing, and photophobia.
- 👁️ Small pupil (miosis) due to iris spasm.
- 🔴 Diffuse redness, often worse at limbus (ciliary flush).
- 🌫️ Cloudy anterior chamber from WBCs/protein (“cells and flare”).
- ⬇️ Visual acuity may be reduced; look for hypopyon.
- 🔍 Posterior synechiae, keratic precipitates, corneal infiltrates may be seen.
- 📏 Always check IOP and corneal staining (exclude keratitis/trauma).
🧪 Investigations
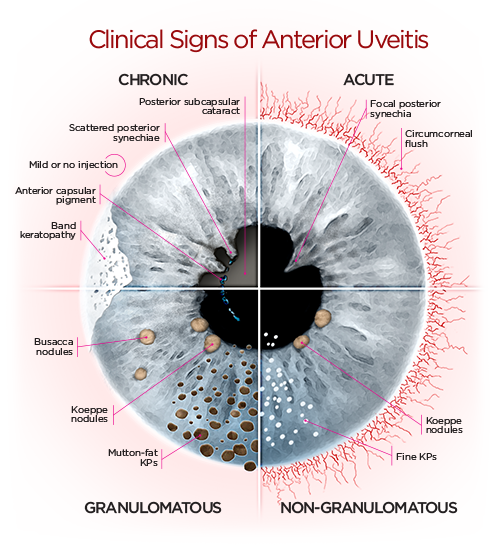
- 🔬 Slit lamp: anterior chamber cells, flare, keratic precipitates (fine = nongranulomatous; “mutton-fat” = granulomatous).
- 🧬 PCR useful in herpetic uveitis/acute retinal necrosis.
- 🩺 Systemic work-up: FBC, ESR/CRP, ANA, HLA-B27, syphilis serology, TB screen, chest X-ray (sarcoid/TB).
- 🖼️ Ocular imaging (OCT, B-scan) for posterior disease.
❓ Differentials
- Endophthalmitis (post-surgery/injection).
- Keratitis (bacterial, viral, chemical burn).
- Acute angle-closure glaucoma.
- Intraocular foreign body.
⚠️ Complications
- Glaucoma (raised IOP).
- Cataracts (from disease or steroid treatment).
- Corneal scarring or band keratopathy.
- Cystoid macular oedema.
- Steroid-related systemic side effects.
💊 Management (Ophthalmology referral essential)
- 📞 Urgent referral if suspected endophthalmitis or corneal involvement.
- 🌿 Idiopathic anterior uveitis:
- Topical corticosteroids (prednisolone acetate) tapered over 4–6 weeks.
- Cycloplegics (homatropine 5%, scopolamine 0.25%, or atropine) → relieve spasm & prevent synechiae.
- Mydriatics (phenylephrine) sometimes used in-office to break synechiae.
- 😎 Sun protection: sunglasses, brimmed hat, dimmed lighting during acute flare.
- 💊 Herpetic anterior uveitis: topical steroids + oral aciclovir 400 mg BD (long-term prophylaxis if recurrent).
- 💉 Severe or posterior uveitis: systemic steroids, immunosuppressants (methotrexate, azathioprine, biologics).
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
