| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Abdominal Pain - Adults
Related Subjects:Acute Cholecystitis |Acute Appendicitis |Chronic Peritonitis |Abdominal Aortic Aneurysm |Ectopic Pregnancy |Acute Cholangitis |Acute Abdominal Pain/Peritonitis |Assessing Abdominal Pain |Penetrating Abdominal Trauma
🫀 Peritonitis is a surgical emergency caused by inflammation of the peritoneum, often due to perforated abdominal organs (e.g., appendicitis, diverticulitis, peptic ulcer, ruptured AAA). ⚠️ Immediate attention to ABC (airway, breathing, circulation) is critical. 🚨 In elderly, immunocompromised, or steroid-treated patients, signs may be subtle or absent. ⏱️ Early diagnosis and surgical intervention reduce morbidity and mortality.
| 🩺 Initial Management Summary |
|---|
|
ℹ️ About
- 🌊 Generalised Peritonitis: Due to perforated viscus → widespread inflammation.
- 🦠 Acute Suppurative: Pus formation from bacterial infection → classic acute abdomen presentation.
🧪 Aetiology
- 🩸 Inflammation of Peritoneum: Triggered by infection, chemical irritation, or trauma.
- ⚠️ Causes: Leakage of gastric contents, bile, blood, or bacteria into peritoneal cavity.
- 🧪 Aseptic vs. Septic: Sterile irritants (bile, acid, pancreatic juice) may become secondarily infected.
📊 Classifications
- ⏱️ Acute vs. Chronic: Acute = emergency; Chronic (e.g., TB) = slow onset.
- 🔍 Primary vs. Secondary:
- Primary = haematogenous spread (e.g., SBP in cirrhosis).
- Secondary = intra-abdominal source (perforated organ, postop leak).
- 🧫 Septic vs. Aseptic: Bacterial vs. sterile causes (e.g., pancreatitis).
🚨 Causes of Acute Peritonitis
- 🍽️ GI perforations: Appendicitis rupture, diverticulitis, perforated ulcers.
- 💚 Biliary/hepatic: Gallbladder rupture, bile leak.
- 🤕 Trauma: Penetrating injuries, anastomotic leaks.
- 👩🍼 Gynaecological: Ectopic pregnancy rupture, pelvic infection.
- 🧴 Spontaneous Bacterial Peritonitis: In cirrhotic ascites.
- 🌍 Infectious: TB, typhoid, dialysis-related peritonitis.
🧫 Microbiology
- Gram−: E. coli, Klebsiella, Bacteroides fragilis
- Gram+: Streptococcus, Enterococcus
- Fungal: Candida (esp. immunosuppressed)
- Chronic: Mycobacterium tuberculosis
🩺 Clinical Features
- 😖 Severe sudden abdominal pain ± shoulder tip pain (diaphragmatic irritation)
- 🤮 Nausea, vomiting, distension
- 🛡️ Rigid “board-like” abdomen, guarding, rebound
- 📈 Fever, tachycardia, hypotension
- 💥 Septic shock in severe cases
🔎 Investigations
- 🧪 FBC (↑WCC), CRP, U&E, LFTs, lactate, amylase, blood cultures
- ❤️ ECG (exclude MI, look for AF/embolus)
- 👩🍼 β-hCG in women of childbearing age
- 🩻 CXR (free air under diaphragm)
- 🖥️ CT (gold standard for diagnosis and localisation)
- 🩺 USS (abscess/biliary pathology)
⚠️ Complications
- 🦠 Sepsis & septic shock
- 🔥 SIRS → ARDS, AKI
- ⛔ Paralytic ileus
- 💔 Multiorgan failure, death
⚡ Acute Abdominal Pain in Adults — Causes, Features, Investigations & Management
Causes of acute abdominal pain can be grouped by system. This table summarises key conditions with their classic presentation, investigations, and first-line management.
| Cause | Clinical Features | Investigations | Management |
|---|---|---|---|
| Appendicitis 🟠 | Periumbilical → RLQ pain, nausea, fever, rebound tenderness | FBC, CRP, urinalysis, US/CT abdomen | IV fluids, antibiotics, appendicectomy |
| Diverticulitis 🟡 | LLQ pain, fever, altered bowel habit | FBC, CRP, CT abdomen with contrast | IV antibiotics, fluids, surgery if perforated/abscess |
| Perforated Peptic Ulcer 🔴 | Sudden severe epigastric pain, peritonitis, rigid abdomen | Upright CXR (free air), CT abdomen | Resuscitation, IV antibiotics, emergency laparotomy |
| Small Bowel Obstruction 🚫 | Colicky central pain, vomiting, distension, constipation | AXR (dilated loops, air-fluid levels), CT abdomen | NG tube decompression, IV fluids, surgery if strangulated |
| Mesenteric Ischaemia ⚡ | Severe pain “out of proportion”, AF history, metabolic acidosis | Lactate, CT angiography | IV fluids, antibiotics, urgent revascularisation/resection |
| Cholecystitis 🟢 | RUQ pain, fever, Murphy’s sign | US abdomen (stones, wall thickening), LFTs | IV antibiotics, fluids, laparoscopic cholecystectomy |
| Cholangitis 🟢 | Charcot’s triad: RUQ pain, fever, jaundice | LFTs (↑ ALP, GGT, bilirubin), US/MRCP | IV antibiotics, ERCP for stone removal |
| Pancreatitis 🔥 | Severe epigastric pain radiating to back, nausea, vomiting | Serum amylase/lipase ↑, CT abdomen for severity | NBM, IV fluids, analgesia, treat cause (e.g., gallstones, alcohol) |
| Renal Colic 💎 | Severe loin-to-groin pain, haematuria, restlessness | Urinalysis, CT KUB (non-contrast) | Analgesia (NSAIDs), fluids, urology referral if obstructed |
| Ruptured AAA 💥 | Sudden severe abdominal/back pain, shock, pulsatile mass | Bedside US (rapid), CT if stable | ABC resuscitation, emergency vascular surgery |
✅ Key Clinical Advice
- Always assess and stabilise with ABCDE before focusing on diagnosis.
- In unstable patients → urgent surgical review, do not delay for imaging.
- Consider broad differentials; elderly and immunosuppressed may have atypical presentations.
💊 Management
- 🔄 Resuscitation: ABCs, O₂, IV fluids, catheter for urine output.
- 💉 Antibiotics: Broad-spectrum IV (e.g., Tazocin ± metronidazole).
- 💊 Analgesia: IV morphine (2.5–5 mg), antiemetics.
- 🥛 NBM: Prepare for surgery.
- 🧑⚕️ Urgent surgical referral: Early laparotomy/laparoscopy.
🔪 Surgical Management
- Indicated for perforated viscus, bowel ischaemia, or generalised peritonitis.
- Procedures:
- Exploratory laparotomy/laparoscopy
- Resection of necrotic bowel, repair perforations
- Peritoneal lavage, drain abscesses
- Continue IV antibiotics post-op.
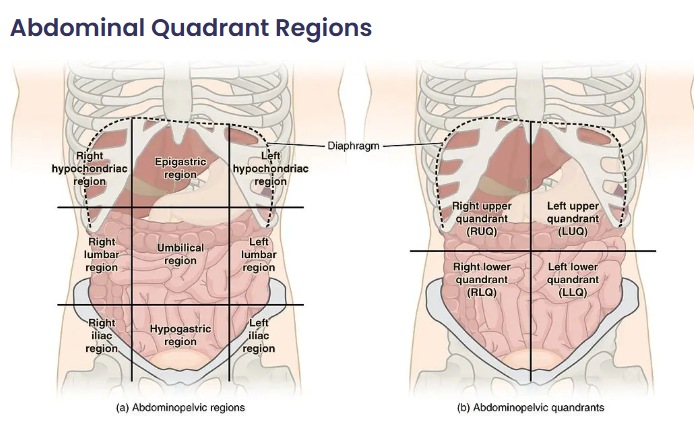
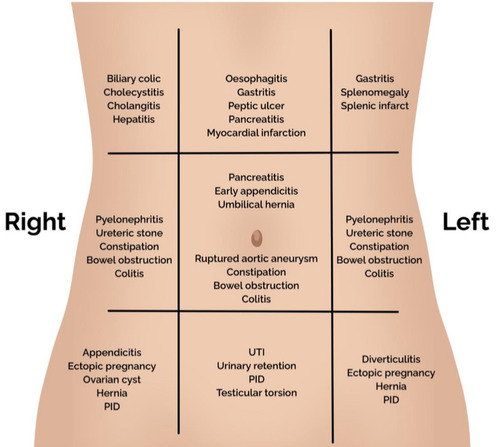
⚡ Acute Abdominal Pain in Adults
Acute abdominal pain is a common emergency presentation. Causes vary by anatomical location. Careful history, examination, and prompt investigations guide diagnosis and management.
| Region & Causes | Clinical Features | Investigations | Management |
|---|---|---|---|
| Right Upper Quadrant (RUQ) 🟢
- Cholecystitis - Cholangitis - Hepatitis - Peptic ulcer perforation |
- RUQ pain ± radiation to shoulder
- Murphy’s sign (cholecystitis) - Jaundice, fever (Charcot’s triad → cholangitis) |
- LFTs (↑ ALP, GGT, bilirubin)
- Abdominal US (gallstones, biliary dilatation) - MRCP/ERCP if obstructive |
- Analgesia, IV fluids
- IV antibiotics (if infection) - Cholecystectomy (definitive for cholecystitis) - ERCP for obstructive stones |
| Left Upper Quadrant (LUQ) 🔵
- Splenic infarct/rupture - Gastritis/peptic ulcer - Pancreatitis |
- LUQ pain ± referred to left shoulder (Kehr’s sign)
- History of trauma (rupture) - Epigastric pain radiating to back (pancreatitis) |
- FBC, amylase/lipase (↑ in pancreatitis)
- CT abdomen (trauma, pancreatitis severity) - Endoscopy (if suspected ulcer/gastritis) |
- Supportive: fluids, analgesia, NBM
- Pancreatitis → IV fluids, monitor severity - Splenic rupture → urgent surgery if unstable |
| Right Lower Quadrant (RLQ) 🟠
- Appendicitis - Mesenteric adenitis - Crohn’s flare - Renal colic |
- Periumbilical → RLQ pain
- Nausea, anorexia, fever - Rovsing’s sign, rebound tenderness |
- FBC (↑ WCC, CRP)
- Urinalysis (exclude UTI/renal colic) - US or CT (appendicitis, renal stones) |
- Appendicectomy (surgical)
- IV antibiotics - Fluids and analgesia |
| Left Lower Quadrant (LLQ) 🟡
- Diverticulitis - Sigmoid volvulus - Colon cancer - Renal colic |
- LLQ pain ± fever
- Altered bowel habit - Abdominal distension (volvulus) |
- FBC, CRP
- CT abdomen/pelvis with contrast (gold standard for diverticulitis) - AXR (coffee-bean sign in volvulus) |
- IV antibiotics, fluids (diverticulitis)
- Endoscopic decompression or surgery (volvulus) - Refer colorectal if malignancy suspected |
| Epigastric/Generalised 🔴
- Perforated peptic ulcer - Pancreatitis - Small bowel obstruction - Mesenteric ischaemia |
- Sudden severe “knife-like” pain (perforation)
- Vomiting, distension (obstruction) - Severe, disproportionate pain (ischaemia) |
- FBC, U&E, lactate (↑ in ischaemia)
- Amylase/lipase (pancreatitis) - AXR/CT (free air, obstruction, ischaemia) |
- ABC resuscitation
- IV fluids, NG tube decompression - Broad-spectrum antibiotics - Emergency laparotomy if perforation or ischaemia |
✅ Key Points
- Always assess ABCDE and resuscitate if unstable.
- Localise pain anatomically to guide differential diagnosis.
- Bloods + Urinalysis + Imaging form the core of investigation.
- Early surgical review is essential for suspected perforation, obstruction, ischaemia, or appendicitis.
📚 References
- Peritonitis: Pathophysiology & Management
- UpToDate: Acute Peritonitis
- Medscape: Peritonitis Overview
Case 1 – Perforated duodenal ulcer
A 48-year-old man with NSAID use develops sudden, severe epigastric pain radiating to the shoulder, rigid abdomen, and absent bowel sounds; vitals show tachycardia, low-grade fever, and mild hypotension. Erect CXR shows free subdiaphragmatic air. Manage with ABCDE, IV fluids, broad-spectrum antibiotics, PPI, NG tube, and urgent CT abdomen; refer for emergency surgery (laparoscopic Graham patch vs definitive ulcer surgery) and test/treat H. pylori after recovery.
Case 2 – Ruptured abdominal aortic aneurysm (AAA)
A 72-year-old man with smoking and hypertension presents with sudden tearing back/abdominal pain, hypotension, and a pulsatile abdominal mass. Avoid excessive fluids (permissive hypotension), give O₂, activate massive haemorrhage protocol, crossmatch, and call vascular surgery for immediate EVAR/open repair. POCUS/bedside ultrasound confirms large infrarenal AAA; do not delay for CT if unstable.
Case 3 – Ruptured ectopic pregnancy
A 30-year-old with 7 weeks’ amenorrhoea and vaginal spotting presents with worsening lower abdominal pain, dizziness, and shoulder tip pain; she is tachycardic and hypotensive with abdominal guarding. β-hCG positive; FAST scan shows free fluid. Resuscitate (O₂, IV access, bloods/crossmatch), consult gynae for urgent salpingectomy (or salpingostomy if appropriate), give anti-D if rhesus negative, and manage pain; differentials include ovarian torsion and ruptured corpus luteum.
Case 4 – Acute appendicitis
A 24-year-old develops periumbilical pain migrating to the RIF with anorexia, mild fever, and rebound tenderness; WBC/CRP raised. Ultrasound (slim female) or CT abdomen confirms inflamed, non-compressible appendix. Give IV fluids, analgesia, and broad-spectrum antibiotics; proceed to laparoscopic appendicectomy. Consider differentials (gynae, mesenteric adenitis); beware atypical retrocaecal pain.
Case 5 – Acute mesenteric ischaemia
A 78-year-old with AF has sudden, severe, diffuse abdominal pain out of proportion to scant early signs; lactate rising, metabolic acidosis. Urgent CTA shows SMA embolus. Resuscitate, start IV heparin and broad-spectrum antibiotics, involve vascular/HPB surgery for embolectomy/revascularisation ± bowel resection if non-viable; mortality is high—act fast.
Case 6 – Sigmoid volvulus
An 82-year-old in a care home presents with abdominal distension, pain, constipation, and tympany; X-ray shows the classic coffee-bean sign pointing to the RUQ. If no peritonitis/ischemia, perform flexible sigmoidoscopy with decompression and rectal tube; arrange definitive surgery (e.g., sigmoid colectomy) due to recurrence risk. If peritonitis or perforation, urgent laparotomy.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
