| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Anatomy of Arteries
Related Subjects: |Anatomy of Skin |Anatomy of the Hand |Anatomy of the Thorax |Anatomy of Muscle Groups |Anatomy of Arteries |Anatomy of the Spinal Column
🩸 A Summary of the Arterial System
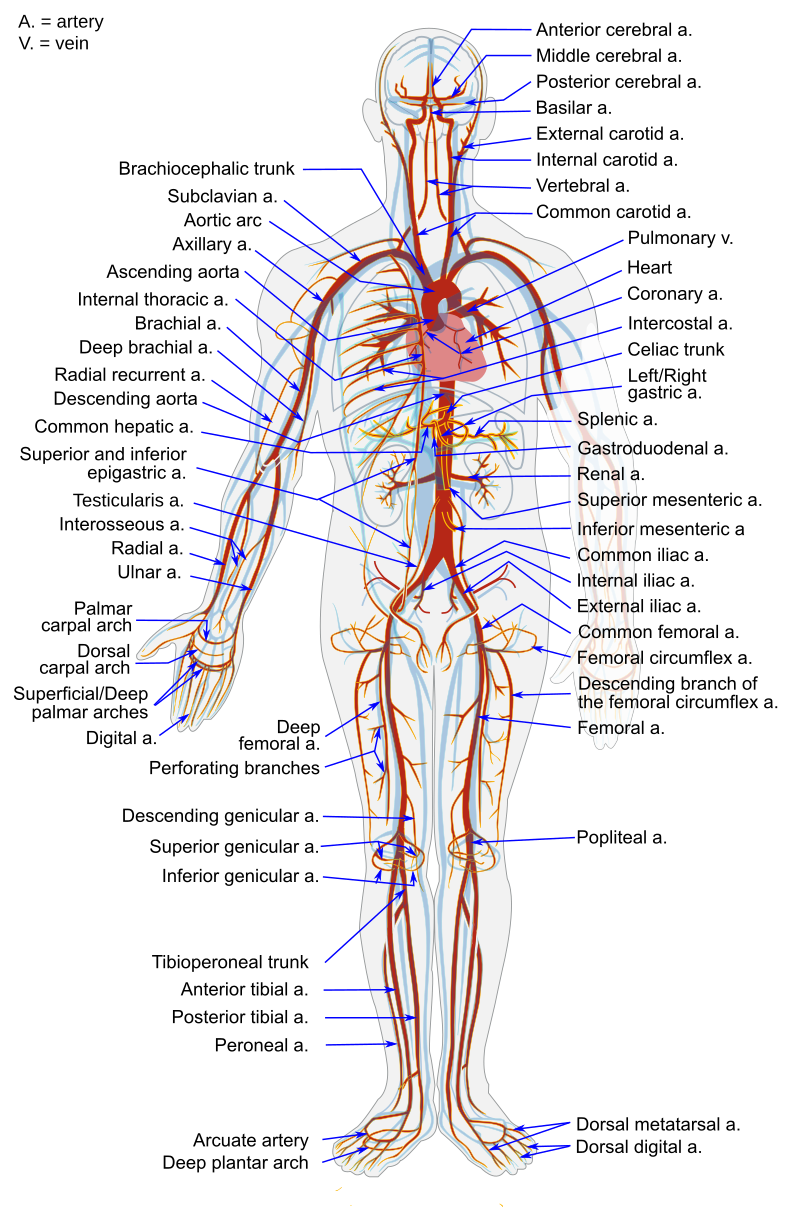
The arterial system forms the high-pressure component of the circulatory network, responsible for delivering oxygenated blood from the heart to every tissue in the body. It begins at the left ventricle with the aorta — the largest artery — and branches extensively into progressively smaller vessels, ultimately forming arterioles and capillary beds. Arteries are structured for strength and elasticity, ensuring efficient perfusion during both systole and diastole. Understanding their anatomy and physiology is crucial for interpreting vascular disease, blood pressure regulation, and systemic perfusion.
🧠 Structure and Function of Arteries
- Tunica intima: The innermost endothelial layer providing a smooth surface to reduce friction; releases nitric oxide (NO) to modulate vascular tone.
- Tunica media: Composed of smooth muscle and elastic fibres — thicker in arteries than veins — allowing constriction (vasoconstriction) and relaxation (vasodilation).
- Tunica externa (adventitia): Connective tissue sheath containing the vasa vasorum (small blood vessels that nourish large arteries) and sympathetic nerves controlling tone.
- Arteries act as pressure reservoirs — their elastic recoil maintains continuous flow during cardiac diastole.
🩺 Classification of Arteries
- Elastic (Conducting) Arteries: Large arteries close to the heart (e.g. aorta, pulmonary arteries, carotids).
- High elastin content buffers pressure fluctuations.
- Their compliance smooths the pulsatile output of the heart into steady flow.
- Muscular (Distributing) Arteries: Medium-sized arteries (e.g. femoral, brachial, coronary).
- Thicker smooth muscle layer allows distribution control to organs.
- Major role in blood pressure regulation.
- Arterioles (Resistance Vessels): Smallest arteries leading into capillaries.
- Major determinant of systemic vascular resistance (SVR).
- Dynamic vasoconstriction and vasodilation regulate blood flow and pressure at the tissue level.
🫀 Major Divisions of the Arterial System
1️⃣ The Aorta
The aorta arises from the left ventricle, ascending before arching and descending through the thorax and abdomen. It divides into several functional sections:
- Ascending Aorta: Gives off the right and left coronary arteries supplying the myocardium.
- Aortic Arch: Curves posteriorly over the left bronchus, giving rise to:
- Brachiocephalic trunk → right subclavian and right common carotid arteries.
- Left common carotid artery.
- Left subclavian artery.
- Descending Thoracic Aorta: Supplies intercostal, bronchial, and oesophageal branches.
- Abdominal Aorta: Extends from the diaphragm (T12) to L4, where it bifurcates into common iliac arteries.
Branches include:
- Celiac trunk → left gastric, splenic, common hepatic arteries.
- Superior mesenteric artery (SMA) → midgut supply.
- Renal arteries → kidneys.
- Inferior mesenteric artery (IMA) → hindgut supply.
- Gonadal arteries → testes or ovaries.
- Lumbar arteries → posterior abdominal wall.
2️⃣ Head and Neck Arteries
- Common Carotid Arteries:
- Right from brachiocephalic trunk, left directly from aortic arch.
- Each bifurcates at C4 into:
- Internal carotid → brain, eyes (via ophthalmic artery).
- External carotid → face, scalp, neck (via facial, maxillary, superficial temporal arteries).
- At the bifurcation lies the carotid sinus (baroreceptor) and carotid body (chemoreceptor).
- Vertebral Arteries: Branch from subclavian arteries, ascend through cervical transverse foramina, entering the skull to form the basilar artery.
- Together, the internal carotid and basilar arteries contribute to the Circle of Willis — a vital collateral network ensuring cerebral perfusion.
3️⃣ Upper Limb Arteries
- Subclavian → Axillary → Brachial → Radial and Ulnar arteries.
- Radial and ulnar arteries form the superficial and deep palmar arches, supplying the hand.
- Brachial pulse (antecubital fossa) and radial pulse (wrist) are key clinical landmarks.
4️⃣ Thoracic and Abdominal Wall Arteries
- Intercostal arteries: Supply chest wall and parietal pleura.
- Internal thoracic artery: Used for coronary bypass grafting due to its longevity.
- Superior and inferior epigastric arteries: Form anastomoses within the anterior abdominal wall.
5️⃣ Lower Limb Arteries
- Common Iliac Arteries: Divide into:
- Internal iliac → pelvic viscera, gluteal region.
- External iliac → continues as femoral artery after passing under the inguinal ligament.
- Femoral → Popliteal → Anterior and Posterior Tibial arteries.
- Dorsalis pedis artery (continuation of anterior tibial) — palpable on dorsum of foot; loss indicates peripheral arterial disease (PAD).
- Posterior tibial artery pulse felt behind the medial malleolus.
🩸 Microcirculation and Arterioles
- Arterioles control flow into capillary beds through precapillary sphincters.
- Autoregulation: Local metabolic factors (e.g. low O₂, high CO₂, low pH) cause vasodilation, enhancing perfusion.
- Systemic control: Mediated by sympathetic nerves (noradrenaline), angiotensin II, and vasopressin (vasoconstrictors); and nitric oxide or atrial natriuretic peptide (vasodilators).
- Pulse pressure depends on stroke volume and arterial compliance.
🧬 Development and Clinical Anatomy
- The arterial system develops from paired embryonic aortic arches; anomalies (e.g. coarctation of the aorta) result from incomplete remodelling.
- Aneurysm: Localised arterial dilation (commonly abdominal aorta at L3–4).
- Atherosclerosis: Intimal lipid accumulation and fibrosis leading to stenosis — clinically presents as angina, claudication, or stroke.
- Arterial pulse examination (carotid, radial, femoral, dorsalis pedis) reflects systemic perfusion.
⚙️ Functional Importance
- Pressure gradient: Maintains continuous blood flow; mean arterial pressure ≈ diastolic + ⅓ pulse pressure.
- Elastic recoil: Converts intermittent ventricular ejection into smooth flow.
- Collateral circulation: (e.g. around joints, Circle of Willis) provides alternative perfusion routes during obstruction.
- End arteries: (e.g. central retinal artery, coronary arteries) lack anastomoses — occlusion causes infarction.
📚 Clinical Correlations
- Arterial Blood Pressure: Determined by cardiac output × total peripheral resistance.
- Pulse Wave Velocity (PWV): Marker of arterial stiffness; increases with ageing and hypertension.
- Peripheral Arterial Disease: Atherosclerotic narrowing of lower limb arteries → intermittent claudication.
- Arterial Cannulation: Common in radial or femoral arteries for monitoring or sampling.
- Aneurysm rupture (especially abdominal aortic) is a vascular emergency; classically presents with back pain, hypotension, and pulsatile abdominal mass.
💡 Key Facts for Clinicians
- The aorta is ~30 cm long and 2.5 cm wide; blood velocity averages 40 cm/s.
- Arteries comprise only ~15% of total blood volume but sustain pressures of 120/80 mmHg systemically.
- The Circle of Willis provides redundancy in cerebral circulation — but ~30% of people have incomplete circles.
- The radial artery is preferred for coronary bypass grafts due to its calibre and muscular wall.
- Arterial compliance decreases with age — leading to systolic hypertension and widened pulse pressure in older adults.
🩸 Teaching Tip: Think of the arterial system as a branching “pressure tree.” The trunk (aorta) stores energy during systole, distributing it through elastic recoil to the branches (arteries) and twigs (arterioles). Pathology anywhere in this system — whether narrowing (stenosis), stiffening (atherosclerosis), or rupture (aneurysm) — has profound systemic effects on perfusion and blood pressure.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
