| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Respiratory Anatomy and Physiology
Related Subjects: Asthma |Acute Severe Asthma |Respiratory Failure |Cardiac Physiology |Renal Physiology |Liver Physiology |Pulmonary Physiology |Pancreas Physiology |Spleen Physiology |Gastrointestinal tract Physiology |Brainstem Physiology |Bone Physiology
 Ventilation-perfusion mismatch increases A–a gradient (normally <2 kPa).
Ventilation-perfusion mismatch increases A–a gradient (normally <2 kPa).
🔎 Lung Anatomy
- Trachea: cricoid → carina (T4/5).
- Right main bronchus = shorter, wider, more vertical → common site of aspiration.
- Pleura: visceral + parietal with thin fluid layer; pain via intercostal & phrenic nerves (referred to chest wall/shoulder).
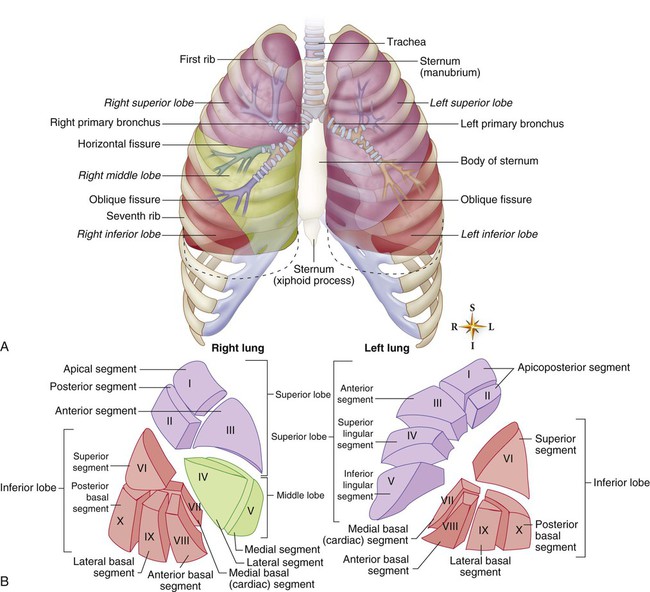
- Lobes: Right = 3 lobes (upper, middle, lower); Left = 2 lobes (+ lingula).
- Bronchopulmonary segments: surgically resectable units with their own artery/bronchus/vein.
📊 Airway Levels
| Trachea → Main bronchi → Lobar bronchi → Segmental bronchi → Small bronchi → Bronchioles → Terminal bronchioles → Respiratory bronchioles → Alveolar ducts → Alveoli |
🔬 Alveolus–Capillary Interface
- Surface area ≈ 90 m²; ~300 million alveoli (diameter <0.2 mm).
- Gas barrier ≈ 0.4 µm (epithelium + BM + endothelium).
- Type I pneumocytes: thin, for gas exchange.
- Type II pneumocytes: secrete surfactant, can differentiate into Type I.
- Surfactant: phospholipid (lecithin, sphingomyelin); lowers surface tension, prevents collapse. Deficiency = neonatal RDS.
🧬 Oxygen–Haemoglobin Curve
- Sigmoid shape due to cooperative binding.
- Left shift: O₂ held tighter (low CO₂, alkalosis, ↓ temp, COHb, fetal Hb).
- Right shift: O₂ released easier (high CO₂, acidosis, ↑ temp, ↑ 2,3-DPG).
- Anaemia (Hb <7 g/dl) → severely limits O₂ delivery.
💨 Oxygen Therapy
- Room air: 21% O₂.
- Nasal cannula: 24–40% FiO₂ (flow-dependent).
- Venturi mask: accurate FiO₂ → best for COPD.
- Non-rebreather: very high FiO₂ (not for CO₂ retainers).
🧠 Respiratory Control
- Central chemoreceptors (medulla): respond to CO₂ via CSF H⁺.
- Peripheral chemoreceptors: carotid body (CN IX), aortic body (CN X) → sense low PaO₂ (<8 kPa), high CO₂, acidosis.
- Sensation of dyspnoea: muscle receptors, J-receptors, chemoreceptors.
- Normal driver: CO₂. In COPD → hypoxic drive can predominate.
🌬️ Causes of Hypoxia
- Normal V/Q ratio ≈ 0.8 (4 L/min ventilation ÷ 5 L/min perfusion).
- PE: V normal, Q ↓ → dead space.
- Pneumonia/asthma: V ↓, Q normal → shunt.
📐 Physics of Respiration
- Dalton’s law: total pressure = sum of partial pressures.
- Atmospheric pressure at sea level = 760 mmHg (101 kPa).
- pO₂ at sea level = 0.21 × 760 ≈ 159 mmHg (21.2 kPa).
- On Everest (252 mmHg): 0.21 × 252 ≈ 52 mmHg (6.9 kPa) → severe hypoxia, needs supplemental O₂.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
