Makindo Medical Notes"One small step for man, one large step for Makindo" |

|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. | |
Haemodialysis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Acute Kidney Injury (AKI) / Acute Renal Failure |Respiratory Failure |Non invasive ventilation (NIV) |Haemodialysis |Cautions Renal Dialysis and Transplant Patients |Continuous Ambulatory Peritoneal Dialysis (CAPD)
Haemodialysis
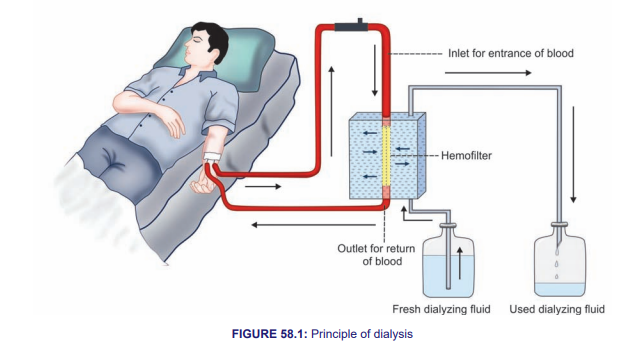
Haemodialysis is a medical procedure used to treat advanced kidney failure. It involves using a machine to filter waste products and excess fluids from the blood, performing the function of the kidneys. Here is an overview of the process, indications, and considerations for haemodialysis.
Indications for Haemodialysis
- End-stage renal disease (ESRD) with typically kidney function is below 15% of normal
- Acute kidney injury (AKI) with severe electrolyte imbalances or fluid overload unresponsive to medical treatment.
- Severe symptoms of uraemia (e.g., nausea, vomiting, fatigue, confusion).
- Refractory hyperkalemia (high potassium levels).
- Refractory acidosis (high levels of acid in the blood).
- Severe Fluid overload resistant to diuretics
The Haemodialysis Process
- Access to Blood :
- Arteriovenous (AV) Fistula : A surgical connection between an artery and a vein, usually in the arm. Preferred for long-term dialysis due to lower risk of infection and clotting.
- Arteriovenous (AV) Graft : A synthetic tube connecting an artery and a vein, used when veins are not suitable for a fistula.
- Central Venous Catheter : A temporary access placed in a large vein, typically in the neck or chest, used for immediate dialysis.
- Dialysis Machine :
- Blood is drawn from the patient’s access site and pumped through the dialysis machine.
- The blood flows through a dialyzer, a filter with a semipermeable membrane.
- Dialysate, a special fluid, flows on the other side of the membrane, allowing waste products and excess fluids to diffuse from the blood into the dialysate.
- Cleansed blood is then returned to the patient’s body.
- Frequency and Duration :
- Typically performed three times a week.
- Each session lasts about 3-5 hours.
Complications and Management
- Hypotension :
- Common during or after dialysis due to rapid fluid removal.
- Management includes adjusting the rate of fluid removal, using midodrine, and ensuring adequate fluid intake.
- Infection :
- Particularly with central venous catheters.
- Prevention includes strict aseptic technique and using antibiotic locks for catheters.
- Access Site Complications :
- AV fistula or graft can develop thrombosis or stenosis.
- Regular monitoring and ultrasound evaluation help detect problems early.
- Electrolyte Imbalances :
- Can occur due to incorrect dialysate composition or rapid shifts during dialysis.
- Regular blood tests and adjustments to dialysis prescriptions are essential.
Advantages and Disadvantages of Haemodialysis
- Advantages :
- Efficient removal of waste products and excess fluids.
- Performed under medical supervision, allowing for immediate management of complications.
- Does not require daily treatment, offering free days between sessions.
- Disadvantages :
- Requires frequent visits to a dialysis center.
- Can cause significant lifestyle disruption.
- Risk of complications such as infection, hypotension, and vascular access issues.
Summary
Haemodialysis is a life-saving treatment for patients with advanced kidney failure. It involves filtering the blood to remove waste products and excess fluids using a dialysis machine. While it is an effective treatment, it comes with potential complications and requires significant lifestyle adjustments. Proper management and regular monitoring are essential to ensure the best outcomes for patients undergoing haemodialysis.